神经退行性病
-
Figure 1|Multiple sclerosis/experimental autoimmune encephalomyelitis immunopathogenesis.
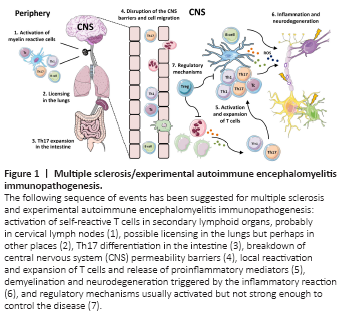
Much of the scientific knowledge concerning the immunopathogenesis of MS derives from investigations performed with EAE. This disease is artificially induced in rodents, mainly mice and rats, by immunization with myelin-derived proteins and peptides in the presence of complete Freund’s adjuvant and pertussis toxin (Robinson et al., 2014; Bjelobaba et al., 2018). Despite clear differences between human and animal diseases (Lassmann and Bradl, 2017), this experimental model is considered suitable for studying MS immunopathogenesis. The main stages of this pathology are briefly outlined in Figure 1.
Figure 2|Immunomodulatory effects of VitD in EAE.

When we tested the effectiveness of VitD administered at different stages of the disease to control paralysis, a clear picture emerged, indicating that the sooner the disease was treated, better was the result. Significant control of disease disability was observed when VitD was provided 1 or 7 days after disease induction, being the earlier even more efficient (de Oliveira et al., 2020; Mimura et al., 2021). However, when therapy was postponed to 10 days postinfection, VitD lost its effectiveness (not shown). The protective outcome coincided with a stabilizing effect on BBB permeability, which is an interesting finding because a turning point in MS development is exactly BBB disruption and the subsequent transendothelial migration of activated leukocytes to the CNS. We verified that VitD stabilizing ability over the BBB is also crucially dependent upon the stage of the disease; only very precocious intervention with VitD can preserve its normal level of permeability (de Oliveira et al., 2020; Mimura et al., 2021). This competence of VitD to stabilize the BBB was already demonstrated in other scenarios, such as in vivo in a hypoxia/reoxigenation model (Won et al., 2015) and in vitro with human endothelial cells (Takahashi et al., 2017). Some of the immunomodulatory effects of VitD in experimental models of MS are depicted in Figure 2.
Figure 3|Effect of precocious and preclinical oral administration of VitD on EAE development.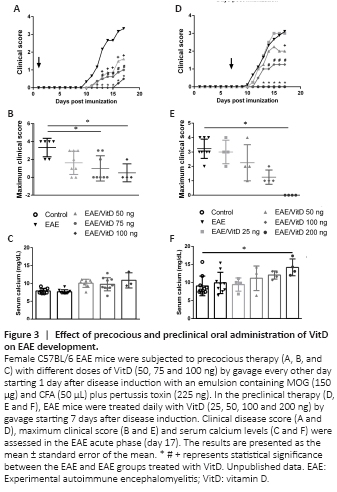
As the results concerning VitD were observed by its intraperitoneal administration, we recently tested its per-oral efficacy. We presumed that this approach could better mimic the physiological immunoregulatory role of this hormone and considered that this is a more friendly procedure that facilitates patient adherence to therapy. As illustrated in Figure 3, per-oral delivery of VitD was also able to control paralysis development when administered 1 or 7 days after disease induction. Interestingly, unlike previous findings that indicated high calcium levels in the blood after delivery of VitD by the intraperitoneal route (de Oliveira et al., 2020), the oral route determined only a nonsignificant increase in serum calcium levels. However, efficacy was again more pronounced when therapy was delivered earlier. Taken together, our results employing the experimental model indicated that VitD administration in the early phase is clearly effective in reducing disease severity. The translation of these and of other authors’ findings to MS patients would require that their future disease development could be already predicted during the prodromal phase. Even though this still seems a challenging task, increasing evidence suggests that MS patients present various clinical manifestations, such as anxiety, depression, migraine, and lower cognitive performance, several years before diagnosis (Giovannoni, 2017; Disanto et al., 2018). According to those authors, the identification of a prodromal syndrome in MS can positively impact patient management.