脑损伤
-
Figure 1|Effect of SGB on infarct volume and eye changes in ischemic stroke diabetic rats.

In this experiment, left SGB was performed using the percutaneous posterior approach after the MCAO model was successfully established (Abdi and Yang, 2005) and slightly adjusted. However, no rats died directly as a result of the SGB operation in this study. The primary surgical procedure was as follows: the MCAO model rats were anesthetized with sevoflurane (3.5% for induction and 2.0% for maintenance) through a face mask and a heating pad was used to maintain the body temperature at 37°C. After the induction of general anesthesia, the rats were connected to anesthesia masks to maintain spontaneous breathing and placed in a prone position. The cartilage of the rat C7 spinous process was palpated as a marker, and a 1-mL syringe with a short, beveled needle was advanced in the anteroposterior direction along the left side of the C7 vertebral body in the median sagittal position. When the needle tip and vertebral body made contact the needle was withdrawn approximately 0.5 mm and the plunger was retracted to confirm that no blood or cerebrospinal fluid was aspirated. Then, a local anesthetic was injected (0.3 mL of 1.0% lidocaine). The above operation was performed on all rats at the same point in treatment by the same experimenter, who was skilled in rat SGB. Once the nerve block was complete, sevoflurane administration was stopped, and the rat regained consciousness after a few minutes. At that time, we observed whether rats had ptosis, and eye fissure reduction (Figure 1A) was considered to judge that SGB was successful (Abdi and Yang, 2005). In addition, we found that the ear capillaries of some rats were dilated after SGB (Additional Figure 2). All groups were operated with SGB apart from the Sham and MCAO groups. The rats were subjected to SGB 15 minutes before reperfusion and again 20 and 44 hours after reperfusion. The time difference between the SGB night group and SGB daytime group operations was 12 hours.
Forty-eight hours after MCAO, the rats in the MCAO group showed prominent infarct areas and the infarct size was significantly reduced after either day or night SGB treatment (P < 0.05) (Figure 1B and C). Consistent results were obtained for brain water content that was significantly reduced after SGB treatment (Figure 1D).
Figure 2|Long-term functional benefit of SGB in ischemic stroke diabetic rats.
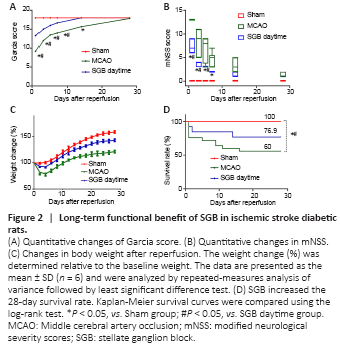
Figure 3|Effect of SGB performed at night or day in ischemic stroke diabetic rat.
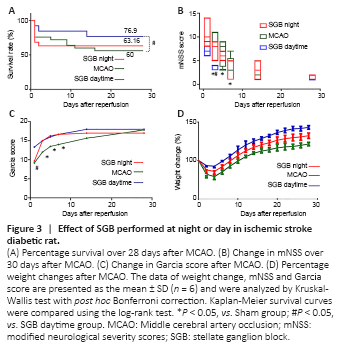
SGB administered in the daytime effectively improves long-term neurological function compared with the MCAO group. There was a significant improvement in the modified neurological severity score and Garcia score in the SGB daytime group, which showed accelerating positive neural outcomes compared with the MCAO group (Figure 2A and B). The postoperative weight changes in the SGB daytime group showed a smaller loss and a more rapid recovery (reaching the lowest value on the third day and returning to the preoperative value on the sixth day) compared with the MCAO group (Figure 2C). SGB was found to confer a significant survival benefit, the MCAO group had a lower 28-day survival rate than the SGB daytime group (P = 0.02; Figure 2D), but there was no significant difference in the survival rate between the MCAO and SGB night groups (P = 0.50; Figure 3A). However, there was some improvement in the long-term neurological functions of the SGB night group (Figure 3B and C). The mean weight in the SGB night group was lowest on day 5 and recovered to baseline on day 10 (Figures 3D), while that of the MCAO group was lowest on day 5 and recovered to baseline on day 11 (Figures 3D). There was also a significant difference in the 48 hours survival rates between the MCAO and MCAO + SGB + LPS groups. Compared with the MCAO group, the MCAO + SGB + LPS group had a higher mortality (P < 0.05; Table 2).
Figure 4|Immunofluorescence and western blot analysis results reflecting the effect of SGB in ischemic stroke diabetic rats.
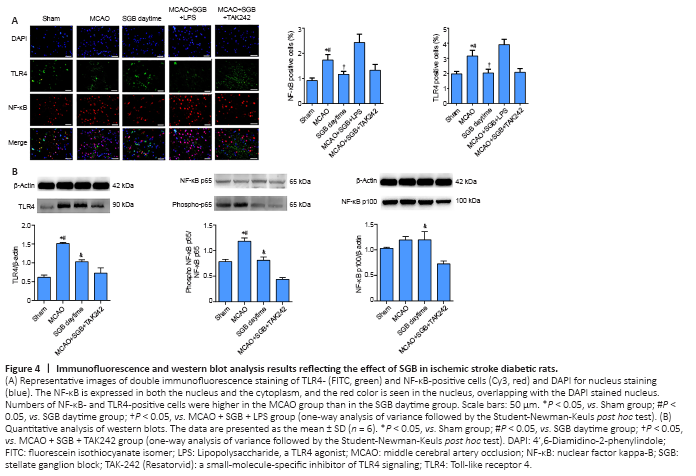
The TLR4 and NF-κB contents were measured by two methods. The localization of the proteins, using immunofluorescence, quantitatively showed that the TLR4 content in the ischemic penumbra of ischemic stroke diabetic rats was greatly decreased when treated with SGB (P = 0.0187; Figure 4A). SGB did not reduce the TLR4 and NF-κB positive cells when administered 5 minutes after LPS (P = 0.0047; Figure 4A). The results of western blot analysis in the ischemic penumbra showed the greatest significant difference (MCAO group vs. SGB daytime group: P < 0.0001; Figure 4B). Immunofluorescence indicated that NF-κB was present mainly in the nucleus in the MCAO group, possibly because nuclear translocation of NF-κB was enhanced in the MCAO group. The western blot results showed that NF-κB p65 phosphorylation was enhanced in the MCAO group, while SGB inhibited this phosphorylation (P = 0.0022). No significant differences in NF-κB p100 phosphorylation were observed, except between the SGB daytime and the MCAO + SGB + TAK242 groups. NF-κB p100 expression in the MCAO + SGB + TAK242 group was significantly lower than that in the SGB daytime group (Figure 4B).