脊髓损伤
-
Figure 3|Combining BMMSC and TMT promotes histological repair of the damaged spinal cord in mice after SCI.
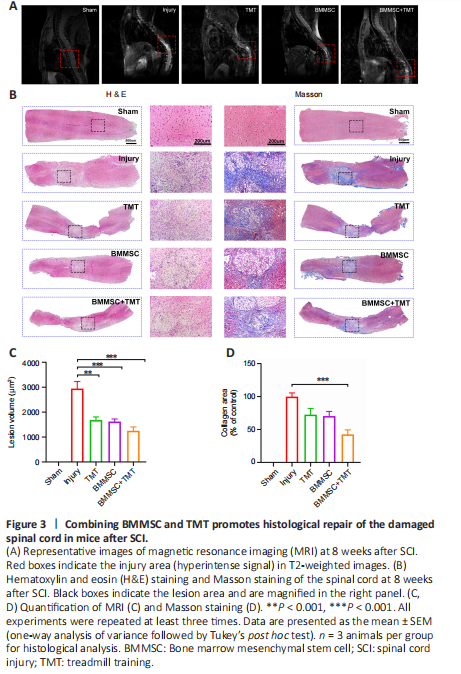
We investigated the effect of the combined therapy on the structural repair of injured spinal cord tissue. The lesion volume of the injured spinal cord was measured at 8 weeks after injury using T2-weighted MRI (Figure 3A). Compared with that in the injury group, a significant reduction in lesion volume was found in mice that received treatment (TMT: P < 0.01, BMMSC: P < 0.001, BMMSC + TMT: P < 0.001; Figure 3C). Nevertheless, the differences between the combined treatment and TMT or BMMSC alone were not statistically significant. The histological changes in morphology in the injured spinal cord at 8 weeks after injury were evaluated using H&E staining (Figure 3B). Severe tissue damage and infiltration of a large number of inflammatory cells were observed in the injury group. After TMT and/or BMMSC treatments, the integrity of the spinal cord was well preserved and the injured tissue showed only mild infiltration of inflammatory cells. Masson’s trichrome staining was also used to estimate scar formation at the site of injury (Figure 3B). TMT or BMMSC alone did not significantly affect the fibrotic area, whereas a significantly lower average percentage of fibrosis was observed in the BMMSC + TMT group than in the injury group (P < 0.001; Figure 3D). These results suggest that TMT or BMMSC alone can promote the preservation of spinal cord tissue, but no significant synergism between them was noted. Furthermore, only the combination of BMMSC and TMT could result in a significant reduction in fibrotic scar formation.
Figure 4|Combining BMMSC and TMT provides neuronal protection and enhances the expression of neurotrophic factors in mice after SCI.
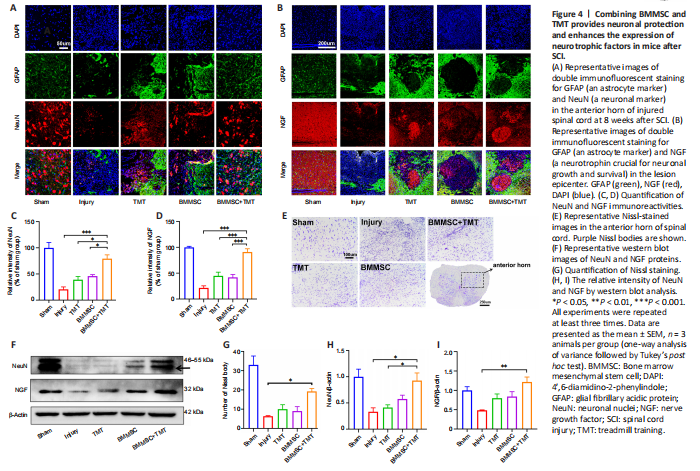
To determine the neuroprotective effect of the intervention on SCI mice, we examined neuronal density in the anterior horn of the injured spinal cord at 8 weeks after SCI by double immunofluorescent staining for GFAP (an astrocyte marker) and NeuN (a neuronal marker) (Figure 4A). SCI induced a significant decrease in NeuN-positive neurons in the anterior horn of the injured spinal cord. The immunofluorescence results showed that the relative density of NeuN in the BMMSC + TMT group significantly increased compared with those in the Injury (P < 0.001), TMT alone (P < 0.05), and BMMSC alone groups (P < 0.05; Figure 4C). However, TMT or BMMSC alone did not significantly affect neuronal viability. We also investigated whether the combination treatment resulted in the enhanced production of NGF, which is a crucial neurotrophin for neuronal growth and survival (Figure 4B). TMT or BMMSC alone did not provide any obvious beneficial effects on NGF production. Only when the two strategies were combined was the NGF level at the injured epicenter region significantly increased compared with that in the injury group (P < 0.001, Figure 4D). For Nissl staining, as shown in Figure 4E, a large number of normal neurons in the sham group displayed an integrative and granular-like morphology, while in the injury group, their numbers were significantly decreased, and most of them exhibited shrunken cell bodies and Nissl granule dissolution. Quantitative comparison of Nissl bodies showed that only the BMMSC + TMT group exhibited a significant increase in the number of surviving neurons compared with the injury group (P < 0.05; Figure 4G). Additionally, western blot analysis of the NeuN and NGF proteins further confirmed the above results (Figure 4F, H, and I). We also detected the protein levels of brain-derived neurotrophic factor (BDNF) and vascular endothelial growth factor (VEGF), but the differences among all groups were not statistically significant (Additional Figure 2). These observations indicated that the combination therapy could exert a protective effect on neurons and promote the repair of damaged tissue after SCI.
Figure 5|Combining BMMSC and TMT promotes axonal and myelin protection in the injured spinal cord in mice after SCI.

The fragmentation of axons at the lesion center of the spinal cord was evaluated by double immunofluorescent staining for GFAP and NF200 (an axonal marker) (Figure 5A and B). GFAP-positive astrocytes accumulated along the lesion border (Figure 5A). Notably, more NF200-positive, injured axons crossed the lesion border in the BMMSC + TMT group than in the TMT (P < 0.05) or BMMSC alone group (P < 0.05) and the injury group (P < 0.05; Figure 5E). In addition, the expression of NF200 in the TMT or BMMSC group was significantly increased compared with that in the injury group (P < 0.05). Double immunofluorescent staining for GFAP and MBP (a myelin marker) was performed to determine the effect of the intervention on remyelination (Figure 5C). We also detected the microstructure of myelin using transmission electron microscopy (Figure 5D). The immunofluorescence results suggested that TMT or BMMSC alone increased the expression of MBP (P < 0.05), but the combination of the two strategies did not result in superior improvement compared with TMT or BMMSC alone (Figure 5F). Furthermore, transmission electron microscopy analysis revealed that only the BMMSC + TMT group had significantly increased myelin thickness, as quantified by the G-ratio, compared with the injury group (P < 0.001; Figure 5G). Moreover, western blot results further confirmed the immunofluorescence findings of NF200 and MBP (Figure 5H–J). Overall, these findings indicate that the combination therapy can alleviate axon and myelin destruction in the injured site compared with TMT or BMMSC alone.
Figure 6|Combining BMMSC and TMT promotes synaptic function in mice after SCI.

Immunofluorescence staining of PSD (a presynaptic marker protein) and SYN (a postsynaptic marker protein) in the injured spinal cord was performed to evaluate synaptic function (Figure 6A and B). The expression levels of PSD and SYN at the injured epicenter region were substantially increased in the BMMSC + TMT group compared with those in the injury group (PSD: P < 0.001, SYN: P < 0.01). TMT or BMMSC alone tended to increase the expression levels of PSD and SYN, but no significant difference was observed between the TMT or BMMSC alone group and the injury group (Figure 6C and D). Western blot analysis for PSD and SYN (Figure 6E–G) also confirmed the above results, indicating that TMT and BMMSC acted synergistically to upregulate the expression of synaptic protein markers better than the individual interventions.