脑损伤
-
Figure 1|Identification and characterization of hDPSCs.

The hDPSCs were adherent and had a typical spindle-like and elongated fibroblastic shape (Figure 1A). Flow cytometry showed that hDPSCs strongly expressed the hDPSC marker CD44, and expressed CD45, the surface antigen of hematopoietic stem cells, at a very low level (0.33%) (Figure 1B). Immunofluorescence staining showed that hDPSCs were positive for CD90, CD105, and CD44, and negative for CD14, CD34, and CD45 (Figure 1C).
Figure 2|MiR-34a expression levels following OGD/R in human dental pulp stem cells and construction of cell groups with miR-34a overexpression and knockdown.

Compared with that in the normal group, cell viability in the hDPSCs with OGD decreased in a time-dependent manner at 12, 18, and 24 hours. We observed no significant difference between the normal group and the hDPSCs that underwent OGD for 6 hours (P > 0.05; Figure 2A). Moreover, we found that miR-34a expression in hDPSCs gradually increased with the extension of OGD treatment time (Figure 2B). To explore the role of miR-34a in hDPSCs, we constructed four cell groups with lentiviral transfection: miR-34a, miR-NC, anti-34a, and anti-NC. The virus vector carried the green fluorescent protein, so successfully transfected cells showed green fluorescence under a fluorescence microscope (Figure 2C). We detected the expression level of miR-34a by RT-qPCR. Compared with that in the anti-NC group, the miR-34a expression level in the anti-34a group was significantly decreased (P < 0.01; Figure 2D). Compared with that in the miR-NC group, the miR-34a expression level in the miR-34a group was significantly elevated (P < 0.01; Figure 2D).
Figure 3|Effects of miR-34a on human dental pulp stem cell apoptosis.

On the basis of previous reports (Zhang et al., 2015; Liu et al., 2018b, 2019) and the above results, we speculated that miR-34a is involved in hDPSC apoptosis. Thus, we detected the expression level of apoptosis-related proteins (Bcl-2 and Bax) in the four cell lines (anti-NC, anti-34a, miR-NC, and miR-34a). The expression level of Bcl-2, an anti-apoptotic protein, was the highest in the anti-34a group and the lowest in the miR-34a group. The expression of Bax, a pro-apoptotic protein, was significantly the lowest in the anti-34a group and the highest in the miR-34a group (Figure 3A). We used TUNEL staining to evaluate the apoptosis rate of the four cell groups. The apoptosis rate was the lowest in the anti-34a group and the highest in the miR-34a group (Figure 3B). Thus, we concluded that hDPSC apoptosis was suppressed by inhibiting miR-34a and aggravated by overexpressing miR-34a.
Figure 4|Effects of miR-34a on the proliferation and antioxidant capacity of hDPSCs.
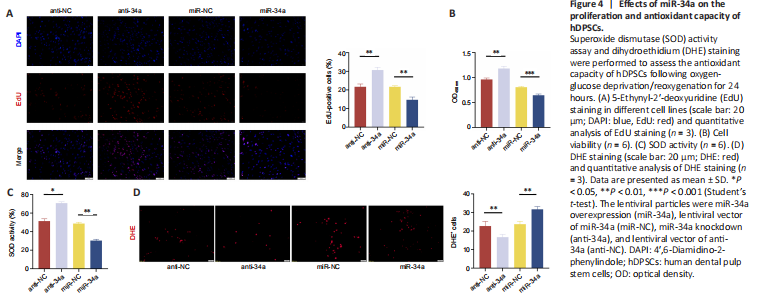
To further explore how miR-34a regulates apoptosis, we detected the cell proliferation and viability of the four cell groups using EdU staining and CCK8 assay. In addition, we used SOD assay and DHE staining to evaluate the antioxidant stress ability of the four cell lines. The proliferation rate and cell activity was significantly increased in the anti-34a group (P < 0.01, vs. anti-NC group) and decreased in the miR-34a group (P < 0.01, vs. miR-NC group) (Figure 4A). Cell activity was significantly increased in the anti-34a group (P < 0.01, vs. anti-NC group) and decreased in the miR-34a group (P < 0.001, vs. miR-NC group) (Figure 4B). SOD activity was significantly increased in the anti-34a group (P < 0.05, vs. anti-NC group) and significantly decreased in the miR-34a group (P < 0.01, vs. miR-NC group). DHE staining showed that the intracellular ROS was significantly decreased in the anti-34a group (P < 0.01, vs. anti-NC group) and significantly increased in the miR-34a group (P < 0.01, vs. miR-NC group) (Figure 4C and D). These results showed that miR-34a inhibition enhanced the proliferation and antioxidant capacity of hDPSCs.
Figure 6|Effects of WNT1 or SIRT1 suppression on apoptosis in miR-34a knockdown cell line.
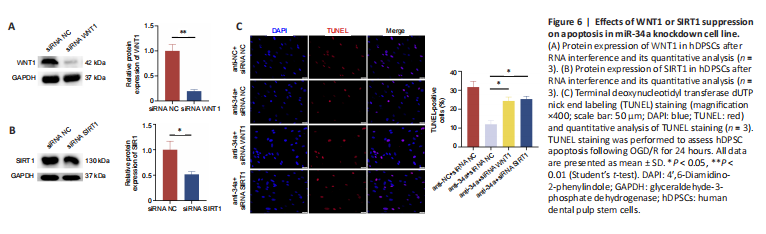
To verify whether the miRNA-34a inhibition exerts an antiapoptotic effect on hDPSCs by targeting WNT1 and SIRT1, we suppressed WNT1 and SIRT1 expression by siRNA in the miR-34a knockdown (anti-34a) cell line. WNT1 protein level was downregulated in the siRNA WNT1 group compared with that in the siRNA NC group (Figure 6A). SIRT1 protein expression was decreased in the siRNA SIRT1 group compared with that in the siRNA NC group (Figure 6B). TUNEL staining showed that the apoptosis rates in the anti-34a + siRNA WNT1 and anti-34a + siRNA SIRT1 groups were elevated compared with that in the anti-34a + siRNA NC group (P < 0.05; Figure 6C). These results indicated that miR-34a inhibition reduced hDPSC apoptosis by targeting WNT1 and SIRT1.
Figure 7|Effects of WNT1 or SIRT1 suppression on the proliferation and antioxidant capacity of miR-34a knockdown in hDPSCs.
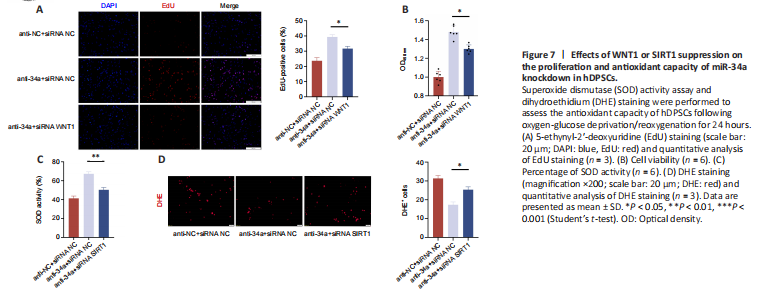
Our previous results showed that miR-34a inhibition promoted the cell proliferation and antioxidant capacity of hDPSCs. Cell proliferation and viability were decreased in the anti34a + siRNA WNT1 group compared with those in the anti34a + siRNA NC group (P < 0.05; Figure 7A and B), indicating that WNT1 suppression partially counteracted the pro-proliferative effect. Similarly, SOD activity was significantly decreased in the anti-34a + siRNA SIRT1 group compared with that in the anti-34a + siRNA NC group (P < 0.01; Figure 7C), indicating that SIRT1 suppression partially counteracted the antioxidative effect. DHE staining showed that intracellular ROS was significantly increased in the anti-34a + siRNA SIRT1 group compared with that in the anti-34a + siRNA NC group (P < 0.05; Figure 7D). These results indicated that miR-34a inhibition promoted cell proliferation by upregulating WNT1 and enhanced the antioxidative capacity by upregulating SIRT1.
Figure 8|Transplanted human dental pulp stem cells exerted neuroprotective effects against ischemic stroke in mice.

To further investigate whether miR-34a knockdown could optimize hDPSC therapy for ischemic stroke in mice, we injected normal hDPSCs and hDPSCs with miR-34a knockdown into the ischemic cortex of mice by stereotactic injection, and then assessed the efficacy of the cellular therapy using HE staining (histopathological damage), TUNEL staining, neurological deficit score, brain water content (brain edema), rotarod test, and infarct volume. HE staining showed that in the sham group, cell nuclei were arranged in an orderly manner. In the I/R + PBS group, cell nuclei were disorganized and lysed, and tissue edema was severe, indicating that the tMCAO model was successfully constructed. The injection of hDPSCs, especially hDPSCs with miR-34a knockdown, significantly alleviated the tissue edema and reduced the lysis of cell nuclei (Figure 8A). In the I/R + PBS group, the apoptosis rate was significantly higher than that in the sham group, I/R + anti-NC group, and I/R + anti-34a group (P < 0.01 for all comparisons). Furthermore, the apoptosis rate of the I/R + anti-34a group was significantly lower than that of the I/R + anti-NC group (P < 0.05; Figure 8B and C). The mNSS score was the highest in the I/R + PBS group, indicating that the neurological injury was the most serious in this group. Compared with that in the I/R + PBS group, the mNSS scores in the I/R + anti-NC group and I/R + anti-34a group were significantly decreased (P < 0.05; Figure 8D). The mNSS score of the I/R
+ anti-34a group was lower than that of the I/R + anti-NC group (P < 0.05; Figure 8D). As shown in Figure 8E, the mice subjected to tMCAO had severe brain edema, which was clearly relieved by the transplantation of hDPSCs, especially hDPSCs with miR-34a knockdown. At 7 days post-operative observation, the rotarod test showed that the time spent on the rotating rod was shorter in the I/R + PBS group than in the Sham group, and time spent on the rod was longer in the I/R + anti-34a and I/R + anti-NC groups than in the I/R + PBS group. The I/R + anti-34a group stayed on the rotating rod longer than the I/R + anti-NC group (Figure 8F). The I/R + PBS group had a larger infarct area compared with the Sham group, and the I/R + PBS group had a larger infarct area compared with the I/R + anti-NC group and I/R + anti-34a group (Figure 8G). The I/R + anti-34a group had a significantly smaller infarct volume than the I/R + anti-NC group (P < 0.05; Figure 8H). These results indicated that hDPSCs ameliorated histopathological damage, neurological deficit, brain edema, and sensorimotor function, and reduced the infarct volume. These effects were further enhanced using the hDPSCs with miR-34a knockdown.