脊髓损伤
-
Figure 1|Experimental design flowchart.
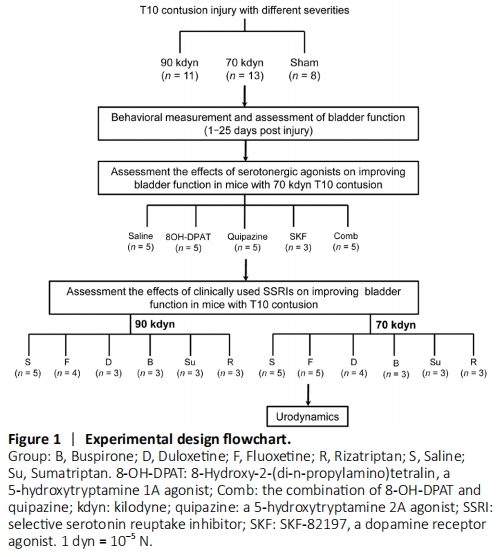
Owing to the technical difficulty of bladder expression following spinal cord injury when using male mice, this study only included female mice. Adult female C57 mice (n = 99), aged 8 weeks, weighing 22–26 g, were obtained from the Laboratory Animal Center of Nantong University in China [license No. SCXK (Su) 2014-0001]. This study was ethically approved by the Institutional Animal Care and Use Committee of Jiangsu Province Hospital of Chinese Medicine (approval No. 2020DW-20-02) on September 11, 2020. All experiments were designed and reported according to the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines. Age- and weight-matched animals were housed at room temperature (22°C) under a standard 12-hour light/dark cycle and were randomly assigned to sham or experimental groups. A flowchart of the experiments, including detailed information regarding the grouping of animals, the numbers of animals in each group, and the varying injury severities that were established, is presented in Figure 1.
Figure 2|Characterization of T10 spinal contusion injury severity.
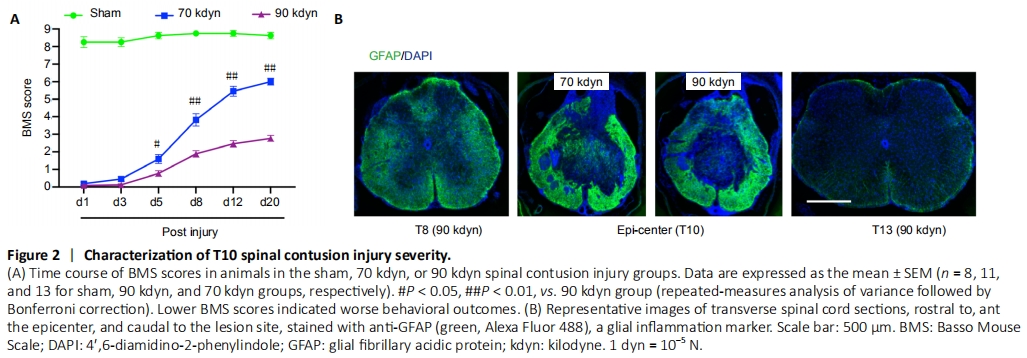
First, we assessed the behavioral outcomes of inducing contusion injuries with different forces. Although in both groups, the BMS scores steadily increased post-injury, the hind limb locomotor recovery was significantly better in the group subjected to moderate force (70 kdyn) compared with the group subjected to a stronger (90 kdyn) force (Figure 2A). At 3 weeks post-injury, the mice in the moderate contusion injury group showed coordinated plantar stepping, achieving a mean BMS score of 6. In contrast, those in the stronger force contusion group only showed occasional plantar stepping, with a mean BMS score of 3 (Figure 2A). Histologically, immunoreactivity against glial fibrillary acidic protein, which serves as a marker for lesion-induced inflammation, showed that the area of the lesion epicenter was smaller in mice from the moderate contusion group (70 kdyn) compared with the group with more severe (90 kdyn) contusion injury (Figure 2B). These results suggested that the moderate contusion injury spared more descending tracts than the severe contusion injury.
Figure 3|Time course of spontaneous voiding recovery following spinal contusion injuries of different severities.

We next assessed the bladder functions of animals following the generation of varying severities of spinal contusion injuries. Consistent with previous studies (David and Steward, 2010), both moderate and severe contusion injuries resulted in compromised bladder function, as indicated by high residual urine volumes. In the moderate contusion group, the volume of expressible urine peaked 4 days post-injury and then declined until reaching a plateau at approximately 12 days post-injury, which remained significantly higher than that for the sham group (Figure 3). In contrast, the residual urine volume of mice in the severe contusion injury group remained high from days 4–20 post-injury (Figure 3), suggesting no spontaneous recovery of bladder function.
Figure 4|Serotonergic receptor agonists increase the voiding efficiency in mice with moderate spinal contusion injuries.
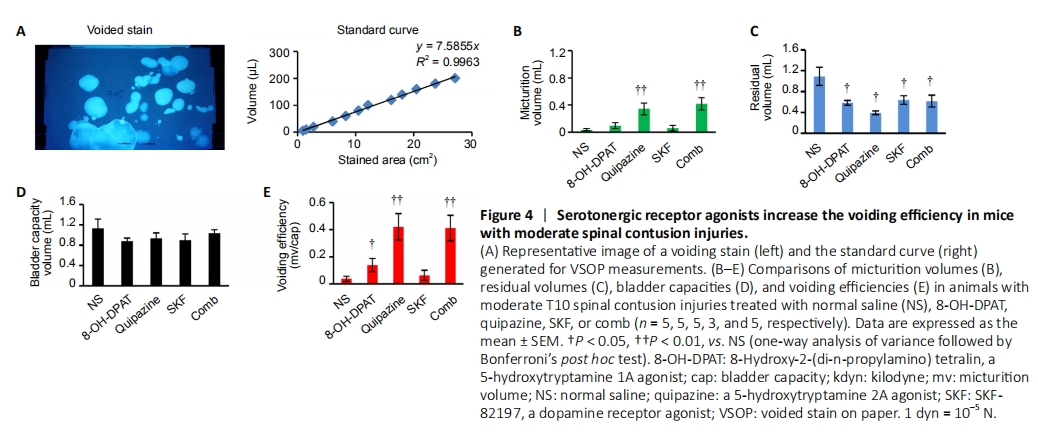
Previous studies suggested that the activation of serotonergic receptors could improve micturition function post-SCI (Dolber et al., 2007; Norouzi-Javidan et al., 2016). To further test this hypothesis, we treated mice with moderate spinal contusion injury with various serotonergic agonists, including quipazine and 8-OH-DPAT, which are both 5-hydroxytryptamine receptor 2A agonist. SKF-8219, a dopamine receptor (D1/D5) agonist, was used as a control. To assess the micturition function, we measured VSOP (Figure 4A). Both quipazine and 8-OH-DPAT significantly improved the voiding efficiency of mice with moderate spinal contusion injury (Figure 4B–E). In contrast, neither normal saline nor SKF-8219 showed any effects (Figure 4B–E), indicating the specific improvement of bladder functional recovery post-SCI in response to serotonergic agents.
Figure 5|Fluoxetine specifically increased the voiding efficiency in animals with moderate T10 spinal contusion injury.
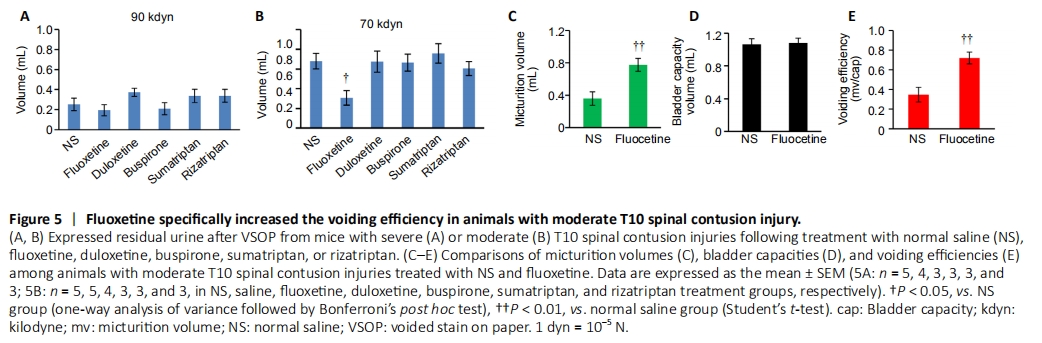
To promote the translatability of this study, we tested the effects of a group of serotonergic drugs that are currently clinically approved. Among these drugs, the widely used selective serotonin reuptake inhibitor (SSRI) fluoxetine increased the voiding volume during the VSOP test, indicating improved voiding efficiency (Figure 5A–E). In contrast, the tested clinically approved serotonergic agonists did not improve micturition function (Figure 5B), likely because of a lack of specificity for the activation of serotonergic supraspinal axons, which is mediated by 5-hydroxytryptamine receptors. Fluoxetine treatment did not have any effects on micturition function in mice with severe spinal contusion injury (Figure 5A), which may indicate that all descending serotonergic axons might be severed.
Figure 6|Urodynamics of mice in sham or moderate T10 spinal contusion injury groups.
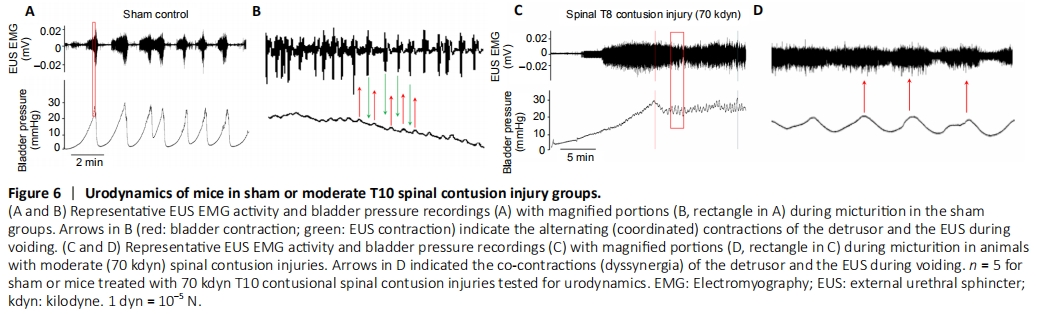
Figure 7|Fluoxetine improves bladder function recovery in mice with moderate T10 spinal contusion injuries.
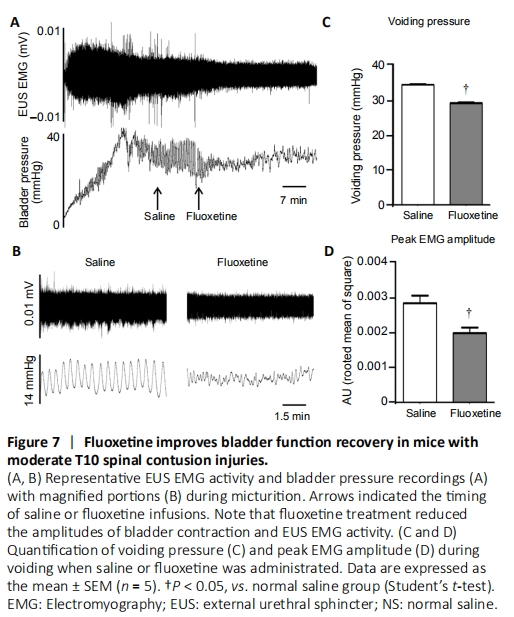
To further investigate the quality of bladder function, we performed urodynamics assessments to measure bladder contractions and EUS activity during voiding in the sham and moderate spinal contusion injury groups. As shown in Figure 6, in the sham group, the EUS showed a basal level of tonic activity. Starting from the onset of voiding, when the bladder pressure rapidly increases, the EUS bursts phasically to coordinate with bladder contractions (Figure 6A and B). In contrast, following moderate spinal contusion injury, animals developed hyperactive, atypical EUS EMG bursting activity during both the non-voiding and voiding periods (Figure 6C and D). The administration of fluoxetine significantly diminished the amplitudes of bladder contractions and EUS EMG bursting activity during voiding (Figure 7A–D). However, we did not observe any overt improvements in coordinated EUS-bladder contractions during micturition. These results suggested that fluoxetine treatment might reduce bladder hyperreflexia and EUS hyperactivation post-SCI.