视神经损伤
-
Figure 1|Scanning electron microscopy picture and corneal histologic section with hematoxylin and eosin staining showing the photodisruption process of femtosecond laser.
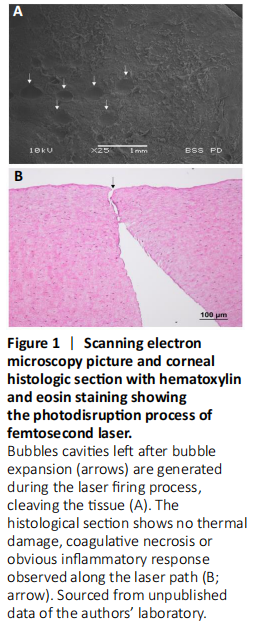
The femtosecond laser (FSL) represents a significant milestone in ophthalmic surgery, including refractive surgery (Liu et al., 2018; Han et al., 2020), keratoplasty (Liu et al., 2019), conjunctival and cataract surgery (Fuest et al., 2017; Liu et al., 2017). The FSL utilizes ultrashort pulses of near-infrared wavelength light to make tissue incisions (Liu et al., 2015). Reducing the pulse duration to a femtosecond (10–15) level produces smaller microcavitation bubbles (Figure 1A) and shock waves, thereby reducing the degree of collateral damage (Figure 1B), which is often associated with conventional lasers such as the argon fluoride excimer laser for photoablation (Liu et al., 2015; Fuest et al., 2017). With an accuracy of 5 μm, the FSL’s ability to photodisrupt tissue with high precision is ideal for surgeries wherein precision is crucial to achieving good outcomes (Liu et al., 2016b).
Figure 2|The neurogenic inflammation process following injury to the cornea.
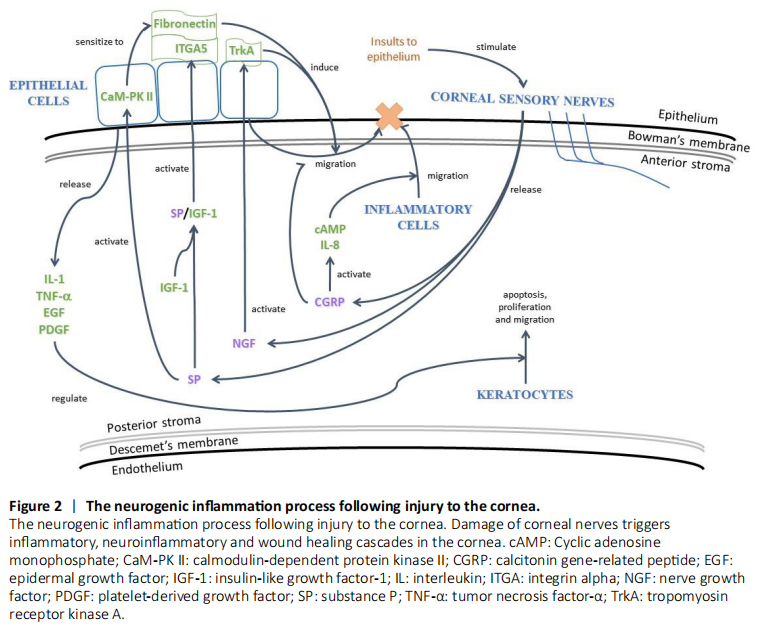
Corneal wound healing is associated with the postoperative refractive stability, predictability, visual outcomes and resultant patient satisfaction following refractive surgery (Liu et al., 2015). The healing process is complex, involving various interactions between cells, neuromediators, cytokines and chemokines on the cornea and ocular surface (Lim et al., 2016; Yawata et al. 2019). In response to stimuli such as FSL ablation or surgical incision, corneal sensory nerves of rats are stimulated to release the neuropeptides SP and CGRP, the principle mediators of neurogenic inflammation (Liu et al., 2020a). In rabbit cornea, SP interacts synergistically with IGF-1 to promote the migration of epithelial cells to the site of tissue injury (Al-Aqaba et al., 2019). Furthermore, through the activation of calmodulin-dependent protein kinase II in rabbit corneal epithelial cells, SP enhances cell migration via the induction of fibronectin and interleukin (IL)-6 (Yamada et al., 2005). Another neuropeptide, CGRP, modulates the innate immune response through the activation of cyclic adenosine monophosphate and IL-8, hence promoting the migration of inflammatory cells such as neutrophils to the wounded site. The epithelium also produces cytokines and growth factors, including IL-1, tumor necrosis factor-α, epidermal growth factor, and platelet-derived growth factor (Mohan et al., 2000). These inflammatory and trophic factors function to regulate apoptosis, proliferation and the migration of keratocytes after laser refractive surgery (Figure 2).