视神经损伤
-
Figure 1|Common routes of cell delivery to the rat retina.
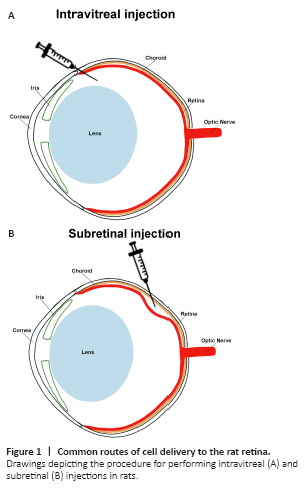
Numerous animal studies have reported that bone-marrow derived cells injected into the eye, both intravitreally and subretinally, may be able to integrate into the retinas and replace dead or defective cells, or release different growth factors leading to increased cell survival, growth and function of resident retinal cells (Wang et al., 2010; Moisseiev et al., 2016), and have also showed in clinical trials some clinical improvement in visual function and absence of severe side effects (Siqueira et al., 2011). The administration route may have a significant impact in the subsequent therapeutic outcomes. Accordingly, intravitreal administration (Figure 1A) of bone marrow-derived stem cells into the vitreous, and thus close to the inner retina, has been shown to delay axotomy-induced RGC loss and to promote neuroregeneration by inducing axon regeneration through increased secretion of trophic factors (Zaverucha-do-Valle et al., 2014). Otherwise, the subretinal administration route (Figure 1B), that delivers bone marrow-derived stem cells closer to the outer retinal layers and thus to photoreceptors, has been described to possess a more direct therapeutic effects on the subretinal space, being therefore considered as a suitable therapeutic alternative for external vitreoretinal disorders (Peng et al., 2017). However, both these routes of administration may occasionally produce some unwanted side events, such as retinal detachment, disturbance of the structures of the retina, intraocular inflammation or ocular hemorrhage (Falavarjani and Nguyen, 2013). Other reported, although less employed, cell delivery strategies include epiretinal, subretinal, retrobulbar and sub-tenon administration and have showed also beneficial therapeutic outcomes in some preclinical and clinical situations (Guan et al., 2013; Tzameret et al., 2015; Weiss and Levy, 2018, 2020, 2021).
Figure 2|Possible mechanisms of action of bone marrow derived-mononuclear stem cells (BM-MNCs).
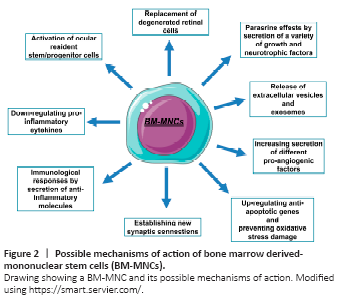
Reported mechanisms of action of allogeneic bone marrow-derived stem cell transplantation include (Figure 2): (i) cell replacement of degenerated retinal cells due to their trans-differentiation properties (Tomita et al., 2002; Chan-Ling et al., 2006); (ii) induction of retinal cell survival and differentiation through their paracrine effects: secretion of growth and neurotrophic factors, i.e., nerve growth factor, brain-derived neurotrophic factor, CNTF, glial cell line-derived neurotrophic factor, transforming growth factor, stem cell growth factor, platelet-derived growth factor, epidermal growth factor, fibroblast growth factor and insulin-like growth factor (Wang et al., 2010; Millan-Rivero et al., 2018); (iii) stimulation of retinal neovascularization by increasing the secretion of pro-angiogenic factors, mainly vascular endothelial growth factor, and thus favoring retinal microhemodynamics (Grant et al., 2002; Otani et al., 2002; Millan-Rivero et al., 2018); (iv) protection of photoreceptors through up-regulation of anti-apoptotic genes (i.e., Mad1, Yy-1, Crybb2, Cryaa and Cryba1 genes) and prevention of oxidative stress damage (Otani et al., 2004); (v) promotion of neuronal rescue by establishing new synaptic connections (Otani et al., 2004); (vi) modulation of host immunological responses: secretion of anti-inflammatory molecules (i.e., transforming growth factor, prostaglandin E2 (PGE2), PGE2 receptor (PGE2R), nitric oxide, interferon and thrombospondin-1 and down-regulation of pro-inflammatory cytokines (i.e., tumor necrosis factor, interleukin-1 and interferon (Millan-Rivero et al., 2018; Hermankova et al., 2019); (vii) activation of ocular stem/progenitor cells (Crisostomo et al., 2008); and (viii) release of extracellular vesicles and exosomes, which contain proteins, mRNA, microRNA, lipids, ribosomes and mitochondria, allowing cell-to-cell communication (Mead and Tomarev, 2017; Seyedrazizadeh et al., 2020). Among all these mechanisms of action, the secretion by bone-marrow derived cells of a variety of molecules with neurotrophic properties has been the most consistent finding in numerous of the above-mentioned studies. These effects have been observed both after intravitreal transplantation of cells into the retina (Millan-Rivero et al., 2018) or even after their intravenous infusion (Wang et al., 2010). The BM-MNCs however, do not seem to integrate within the retina and replace the degenerated cells. As noted above (see section Bone marrow-derived stem cells therapies for degenerative retinal disorders), the whole BM-MNCs fraction contains a heterogeneous population of cells and, although it contains a small proportion of pluripotential cells that could in theory migrate into the retina, the majority tend to differentiate into mesodermal tissues (Fafian-Labora et al., 2015; Wang et al., 2020). Therefore, it is widely accepted that the adult retina is not as receptive to the integration of donor cells as previously thought and that the production of neurotrophic factors by the BM-MNCs is probably the main mechanism of action of the transplants and not cell integration and differentiation.