NRR:中南大学湘雅医院夏健团队发现脑梗死后出血转化的新生物标志物
撰写:黄琴,韦珉坪,封献敬,罗云芳,刘运海,夏健
研究表明,脑卒中是全球第二大死亡原因,我国脑卒中的发病率在过去20年呈现明显上升趋势,是全球卒中发病人数最多的国家[1]。梗死后出血转化 (Hemorrhagic transformation, HT)是指脑缺血区重新恢复血流灌注导致的出血, 根据影像特点分型分为出血性脑梗死(Hemorrhagic infarction, HI)和脑实质出血 (Parenchymal Hematoma, PH),是缺血性脑卒中的常见并发症[2]。出血转化的发生与卒中的严重程度、梗死面积、抗栓药物的使用等密切相关,其中应激性高血糖是梗死后出血转化风险增加的独立危险因素[3]。既往研究表明梗死后出血转化的病理改变与血脑屏障通透性增加及脑水肿等相关,其机制涉及再灌注损 伤、凝血功能异常及氧化应激等,使机体处于促炎、促凝和氧化应激状态[4]。梗死后出血转化是导致卒中患者不良预后的重要原因,目前尚缺乏有效的防治措施[5]。因此,寻找早期预测梗死后出血转化和有效遏制出血转化的新靶点已成为亟待解决的问题。
近日,中南大学湘雅医院夏健团队在《中国神经再生研究(英文版)》(Neural Regeneration Research)上发表了题为“Hemorrhagic transformation in patients with large-artery atherosclerotic stroke is associated with the gut microbiota and lipopolysaccharide”的文章。研究发现,梗死后出血转化促进肠道菌群紊乱,使肠杆菌科相对丰度升高, 致病代谢产物脂多糖 LPS 增加,促进肠脑屏障通透性改变,影响梗死后出血转化的发生发展。该研究为梗死后出血转化提供了新的生物标志物,为可能的作用靶点提供了新的依据。黄琴为论文第一作者,夏健教授为论文通讯作者。
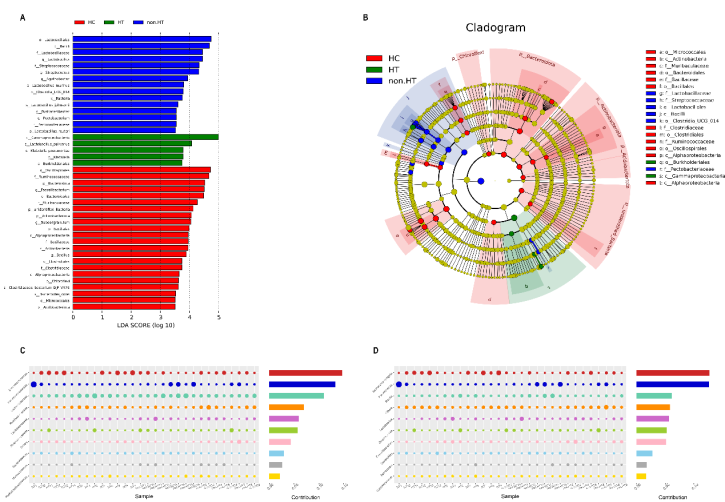
该研究共纳入48名受试者,其中急性大动脉粥样硬化型卒中患者伴有出血转化15例(HT组),卒中后无出血转化17例(non-HT组),以及由16名年龄性别相匹配的受试者作为健康对照组(HC组)。收集患者入院后48小时内的大便标本,运用16sRNA测序对3659508个片段进 行了去噪、合并和存活嵌合滤波,每个样本的读取次数平均为83316次。通过线性判别分析(>3.5)筛选造成各组别差异最明显的肠道菌群。该研究发现,健康对照组存在更多的抗炎型肠道微生物,包括Ruminococcaceae, Acidobacteriota 和 Faecalibacterium ; non-HT 组 的 患 者 存 在 更 高 水 平 的 Streptococcus,Fusicatenibacter 和 Pectobacterium, 在HT组的患者伴有 Lactobacillus_salivarius和Klebsiella的相对丰度升高(图1A和1B)。该研究 也进行了相似度百分比分析(SIMPER),发现肠杆菌科(Enterobacteriaceae)和志贺菌属(Escherichia-Shigella)是造成HT和non-HT组间主要差异的肠道微生物 (图1C和1D)。这两种肠道微生物是LPS产生的主要来源,这提示肠道菌群及其代谢产物LPS可能参与调节梗死后出血转化的发生发展。
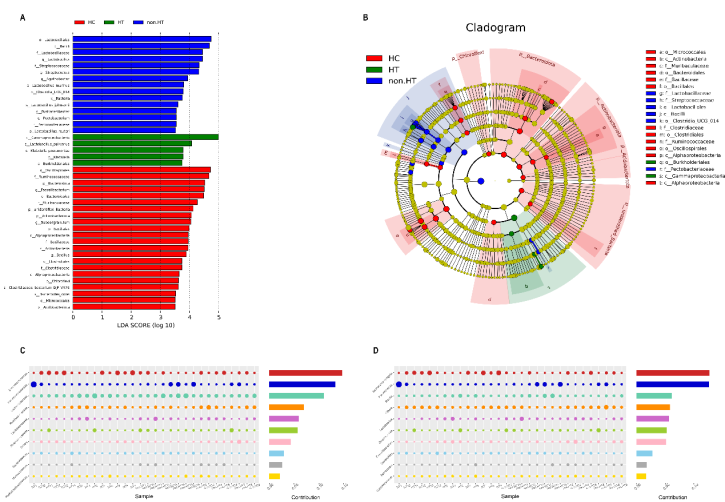
图1 线性判别分析差异肠道菌群造各组别中的分布。(图源:Huang Q, et al., Neural Regen Res, 2023)
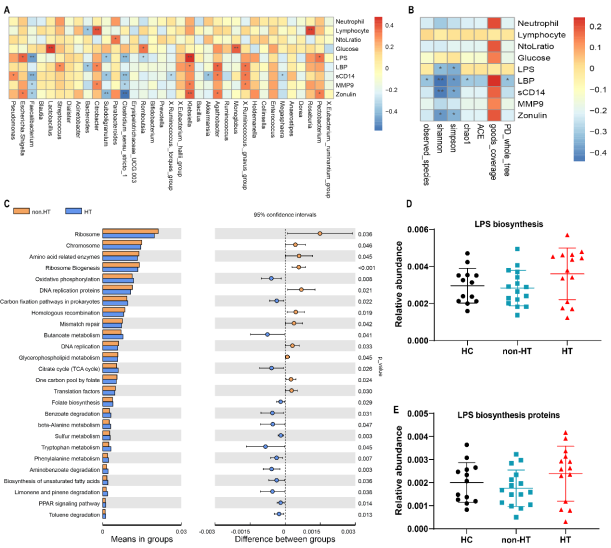
运用spearman分析发现,出血转化临床生物标志物与肠道菌群存在明显的相关性。血浆LPS (r=0.382, p=0.012)和人连蛋白(r=0.323, p=0.034)水平与大肠杆菌、 志贺氏菌的相对丰度呈正相关(图2A)。此外,本研究发现alpha多样性与LPS、 LBP之间存在显著的相关性(图2B)。肠屏障指标人连蛋白的浓度与Simple、 Shannon指数呈负相关(图2B)。因此肠道菌群及LPS参与梗死后出血转化的病理生 理过程。最后运用PICUSt预测差异肠道菌群的功能,总共有97个肠道菌群基因通 路在有出血转化和无出血转化中存在差异,其中83个通路上调,14个基因通路下 调(图2C)。参与氧化磷酸化和不饱和脂肪酸生物合成的基因上调,这些都与心 血管疾病和卒中有关,与LPS相关的PPAR信号通路在HT组也上调。该研究也观察 到,与HC和non-HT组相比,HT组的LPS相关功能通路(LPS生物合成和LPS生物合成 蛋白)呈升高趋势(图2C和图2E)。
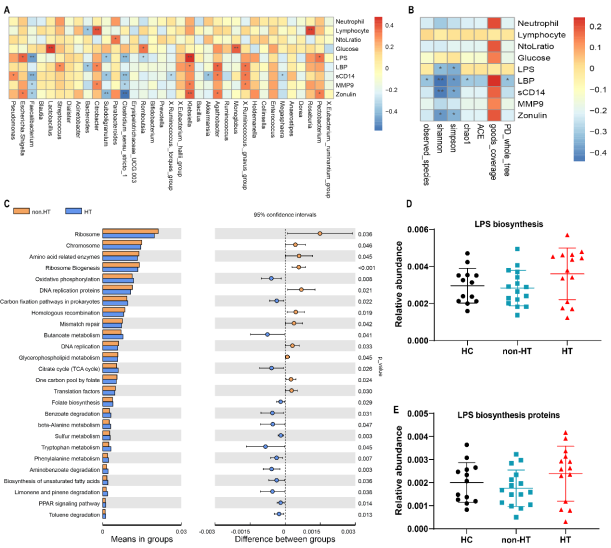
图2 差异肠道菌群基因通路改变情况。(图源:Huang Q, et al., Neural Regen Res, 2023)
为了确定肠道菌群和脂多糖相关炎症反应在HT过程中的作用,该研究构建了梗死后出血转化大鼠模型,并进行了粪菌移植实验。研究发现,相对于移植无出血转化供体的 肠道菌群而言(F-non-HT组),移植出血转化供体的肠道菌群可以增加受体(F-HT组)大鼠的梗死体积和出血转化严重程度(图3A-3C)。出血转化供体来源的微生物群使受体大鼠血浆中存在较高水平 的LPS (p < 0.01)、LBP (p=0.022)和sCD14 (p < 0.01)。

图3 粪菌移植后受体MCAO大鼠脂多糖相关信号的变化。(图源:Huang Q, et al., Neural Regen Res, 2023)
该研究通过临床队列发现梗死后出血转化导致肠道菌群紊乱,肠杆菌科相对丰度增加,致病代谢产物LPS及相关受体LBP、sCD14升高,进一步通过动物实验证实肠道菌群及LPS水平升高,肠脑屏障受损,这可能是影响梗死后出血转化发生的重要因素。
原文链接:https://doi.org/10.4103/1673-5374.385846
参考文献
[2] Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394-405.
[3] Zhang J, Yang Y, Sun H, et al. Hemorrhagic transformation after cerebral infarction: current concepts and challenges. Ann Transl Med. 2014;2(8):81.
[4] Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
[5] Vancheri F, Curcio M, Burgio A, et al. Impaired glucose metabolism in patients with acute stroke and no previous diagnosis of diabetes mellitus. QJM. 2005;98(12):871-878.
[6] de Courten-Myers GM, Kleinholz M, Wagner KR, et al. Fatal strokes in hyperglycemic cats. Stroke. 1989;20(12):1707-1715.