脊髓损伤
-
Figure 1|Study timeline and model of the root magnetic stimulation (NRMS) treatment.
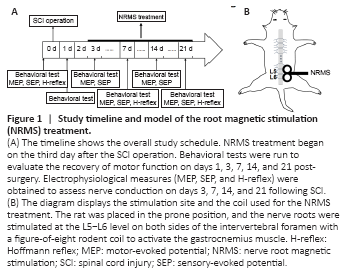
The rats’ locomotor function was assessed at different time points using the Basso-Beattie-Bresnahan (BBB) scale (Basso et al., 1996), the inclined plane test (Duan et al., 2018), the rotarod test (Sauer et al., 2017), and the modified Tarlov score (Jiang et al., 2016). These were run the day before surgery and on days 1, 3, 7, 14, and 21 after surgery (Figure 1). To enable the rats to adapt to the tests, they were run five times before the official tests took place. Each measure was blindly and independently assessed by two observers, and the average scores were recorded for each rat. All of the tests were run on all 15 rats in each group.
Figure 2|Repetitive magnetic stimulation of the nerve root improves motor function in rats with spinal cord injury (SCI).

All 45 SD rats completed the whole battery of behavioral tests assessing motor function. The scores on the tests prior to surgery did not differ significantly between the three groups (P > 0.05; Figure 2). On the first day post-surgery, all of the measures (the BBB score, the inclined plane angle, the on-rod time, and the modified Tarlov score) were significantly lower in the SCI + SS group and the SCI + NRMS group compared with the sham + SS group (P < 0.001; Figure 2). On the third day following SCI, there were no significant differences between the SCI + SS group and the SCI + NRMS group (P > 0.05; Figure 2); however, on the seventh day following SCI, the BBB score, the inclined plane angle, and the on-rod time were all significantly higher in the SCI + NRMS treatment group compared with the SCI + SS group (P = 0.0036, P = 0.0019, and P = 0.0257, respectively; Figure 2). By the end of the second and third weeks, remarkable group differences could be observed for all four tests, with the rats in the SCI + NRMS group having higher scores than the SCI + SS group (P < 0.001 for all tests; Figure 2). These results imply that NRMS treatment leads to improved recovery of locomotor function following SCI.
Figure 3| Effects of nerve root magnetic stimulation (NRMS) on spinothalamic nerve conduction in the spinal cord injury (SCI) rats.
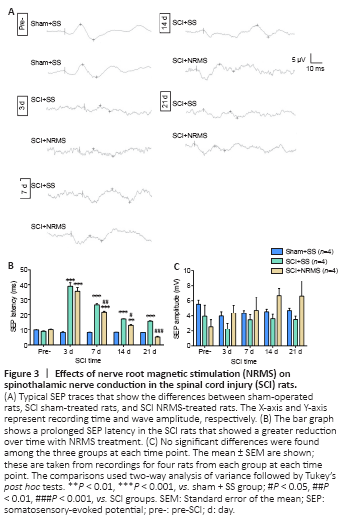
Prior to surgery, there were no significant differences between the three groups in terms of both the latency and amplitude of the SEP. On the third day following surgery, the two groups of SCI rats were found to have prolonged SEP latencies compared with the sham + SS group (P < 0.001; Figure 3A, B), whereas no significant differences were observed between the two SCI groups; there were no significant differences in the SEP amplitudes between the three groups (P > 0.05; Figure 3A, C). After the first week, the SEP latencies in the SCI rats gradually decreased, with a greater reduction seen in the NRMS-treated SCI rats (two-way analysis of variance with Tukey’s post-hoc test: P7 d = 0.004, P14 d = 0.0137, P21 d < 0.001). However, there were no significant differences in the SEP amplitude between the two SCI groups during the study period (P > 0.05).
Figure 4|Effects of nerve root magnetic stimulation (NRMS) on corticospinal nerve conduction in the injured spinal cord of rats.

Prior to SCI surgery, there were no significant MEP latency differences between the three groups of rats. On the third day after surgery, the SCI rats had decreased MEP amplitudes and significantly prolonged MEP latencies compared with the rats in the sham + SS group (Figure 4A–C); there was no significant MEP latency difference between the SCI + NRMS and SCI + SS groups (P > 0.05). For the later time points, the NRMS treatment was found to attenuate the prolonged MEP latency (two-way analysis of variance with Tukey’s post hoc tests: P7 d = 0.0023, P14 d < 0.001, P21 d < 0.001), thus indicating that it induces elevated excitability in the corticospinal tract.
Figure 5| Effects of repetitive magnetic stimulation of the nerve root on peripheral nerve conduction in the injured spinal cord of rats.

The H-reflex recordings (Figure 5A) revealed that there was a significantly longer H-waveform latency in the SCI + NRMS group compared with the SCI + SS group 1 week after surgery (P < 0.01; Figure 5D). For the H-waveform amplitude, although there were noticeable differences between the two groups, this was only significantly different at the end of the first week (P < 0.01; Figure 5C). For the H/M ratio, the percentage of excited alpha motor neurons responding to the electrical stimulation decreased noticeably in the SCI + NRMS group compared with the SCI + SS group on the seventh day after surgery (P < 0.001; Figure 5B), as well as on day 21 after surgery (P < 0.001; Figure 5B).
Figure 6| Effects of nerve root magnetic stimulation (NRMS) on the ultrastructure of synapses in the sensorimotor cortex of rats with spinal cord injury (SCI).

The synaptic ultrastructure in the sensorimotor cortex was examined to determine the effect of NRMS on structural plasticity in the sensorimotor neural pathways. In the SCI + SS group, we observed marked damage to the ultrastructure of the synapses, with a flat synaptic morphology (see triangle symbol in Figure 6A), fewer synaptic vesicles, and more vacuoles than in the sham + SS group. For the SCI + NRMS group, the synaptic structure was closer to normal compared with the SCI + SS group, thus suggesting that there had been a certain amount of recovery to restore the synaptic damage. The significant changes in synaptic ultrastructure that followed SCI included the thickness of the PSD, the length of the synaptic active zone, and the curvature of the synaptic interface (P < 0.001; Figure 6C–E), but not the width of the synaptic cleft (P > 0.05; Figure 6B). Importantly, the length of the synaptic active zone increased substantially with NRMS treatment (P < 0.001; Figure 6D).