周围神经损伤
-
Figure 2 | Axon regeneration and vascularization 7 weeks after surgery using ANT, silk+ tNGCs or silk– tNGCs to treat an 8-mm sciatic nerve defect.
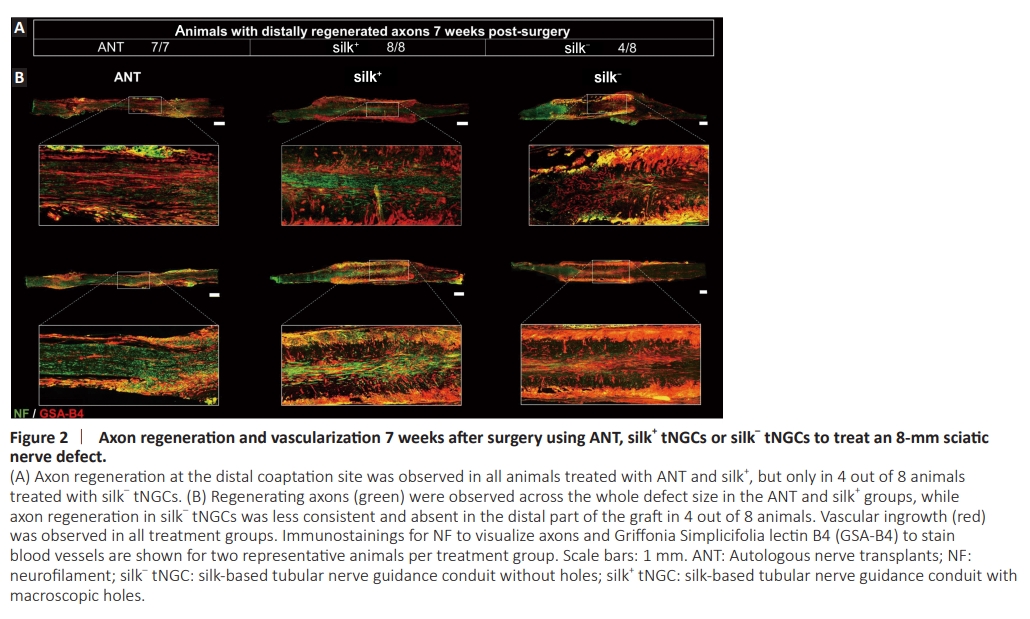
To investigate whether the generation of periodically arranged macroscopic holes in the tubular walls of silk tNGCs enables vascular ingrowth from the surrounding tissue into the lumen, thereby leading to improved nerve regeneration, we first reconstructed an 8-mm sub-critical sciatic nerve defect with either an ANT (Figure 1D), a silk– tNGC (silk– ; Figure 1E), or with a silk+ tNGC (silk+ ; Figure 1F). We compared axon regeneration as well as blood vessel formation 7 weeks after grafting. Regenerated axons at the distal site of the conduit were present in all animals treated with ANT as well as silk+ tNGC, but only in half of the animals with silk– tNGC (Figure 2A). Immunohistochemical evaluation of longitudinal sections of the whole regenerated nerve segments revealed dense axon bundles spanning the entire nerve segments in the ANT and silk+ groups, which were superior to the silk– groups (Figure 2B). Additionally, although vascularization was observed in all groups, blood vessels appeared to grow from and/or to the conduit walls of silk+ grafts (Figure 2B).
Figure 3 | Vascularization using silk+ tNGCs.

Since we could observe at the time of excision of the constructs that blood vessels grew through the holes in the conduit wall (Figure 3A), we also aimed to visualize the blood vessels inside silk tNGCs. Therefore, we perfused the conduits with Lugol’s iodine and Micropaque and performed a microCT scan 7 weeks postoperatively. Blood vessels from the surrounding tissue were seen to have migrated through the tubular wall and anastomosed with blood vessels present in the lumen of the silk+ tNGC (Figure 3B–E). Furthermore, to assess whether the silk+ tNGCs promote vascularization of the regenerating nerve tissue, we quantified the number of vessels present in ANTs, silk– and silk+ tNGCs (Figure 3F and G). Vessel quantification revealed a significantly higher number of blood vessels in the silk+ group compared with ANTs (P = 0.0057) and unmodified silk– tNGCs (P = 0.0292; Figure 3G).
Figure 4 | microCT scans of Lugol’s iodine-stained silk–based tNGCs in comparison with histology.

For a more detailed analysis of these newly formed blood vessels, we compared microCT scans of Lugol’s iodine–stained whole regenerated nerve fragments inside the silk tNGCs with histological stainings (Figure 4). Blood vessels grew from the nerve stumps into the center of the lumen of the silk+ as well as unmodified silk– tNGCs (Figure 4A–D). Vascularization seemed to be enhanced within the silk+ tNGCs with blood vessels growing through the holes, laser-ablated into the tubular walls (Figure 4H). In contrast to our initial hypothesis, blood vessels did not seem to grow from the surrounding tissue into the tNGCs, but rather grew from the central blood vessel inside the lumen to the outside (Figure 4C and D). Corresponding blood vessels in microCT slices and histological longitudinal and cross-sections are highlighted by color-coded circles (Figure 4E–H).