颅神经损伤
-
Figure 1|Flow diagram, consort flowchart for participant recruitment and allocation.
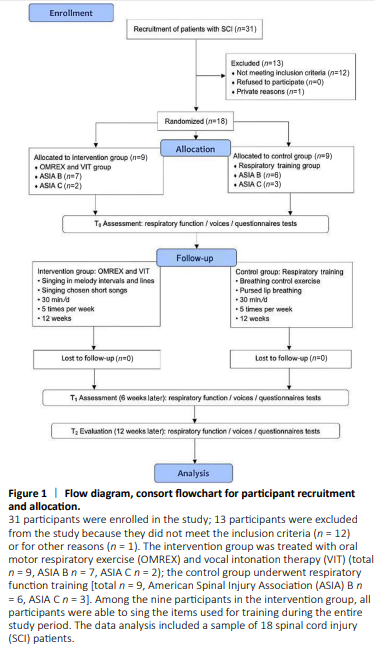
After obtaining approval from the Scientific Research Foundation of the China Rehabilitation Research Center, participants were first screened by SCI specialists. Patients diagnosed with ASIA classification B and C conditions who had respiratory dysfunction were referred to the Music Therapy Department. Participants were reviewed by the researchers to identify potential interventional objectives based on the inclusion and exclusion criteria of the study. Once potential participants were identified, an invitation to the study was sent to the potential participants or to the family members of participants who were not able to make decisions themselves with an explanation of the study, including the purpose, procedures, risks, benefits, confidentiality, and subjects’ rights. Once consent forms were acquired, the participants were divided into two groups based on their ASIA classification. Music therapy researchers screened patients based on previous tracheotomy outcomes to determine whether the patients had abnormal articulation or impaired laryngeal function. After screening, computer-generated sequences (Excel 2013, Microsoft Office software, Seattle, WA, USA) were used to randomly assign patients to the two groups using a completely randomized design. The participants in the intervention group were trained by music therapists for 12 weeks to perform OMREX + VIT, while participants in the control group were trained in respiratory exercises for 12 weeks. The enrollment and allocation of participants are shown in Figure 1.
Once the participants for each group were identified, an intervention delivery schedule was developed. The intervention group was trained in OMREX to improve respiratory volume and was trained in VIT to improve vocal quality by music therapists. Each patient was trained by a music therapist for 30 minutes per session, five sessions a week, for 12 weeks. In the first 10 minutes, the music therapist helped participants to practice inhalation and exhalation on one long single note (Additional Figure 1 bars 1–8) and staccato singing in short melodic intervals as preparation for the session (Additional Figure 1 bars 9–12). In the next 15 minutes, the patient performed vowel singing by melody intervals with alternating tonality practice (Additional Figure 1 bars 13–16), and then a short melody line consonant with alternating tonality practice was performed (Additional Figure 1 bars 17–21). In the last 5 minutes, the patient sang specific Chinese song tracks, such as “Orchid”, “Hawthorn Tree”, or “Country Road”. The control group received routine respiratory function training by a respiratory therapist, including breathing control and pursed-lip breathing (Clini et al., 2018). The therapy sessions of the two groups were both 30 minutes per day, five times a week, for a total of 12 consecutive weeks. All patients underwent routine treatment during the study period. The routine treatment included taking regular medications and other routine care and support.
Figure 3|Comparison of vocal quality in spinal cord injury patients undergoing oral motor respiratory exercise and vocal intonation therapy or respiratory training.
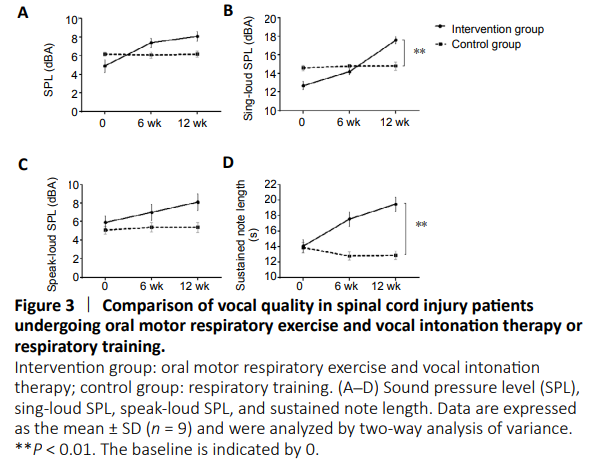
Compared with the control group, the sing-loud SPL (t2 = 17.6 ± 2.1 dBA, F = 7.828, P = 0.0011) and sustained note length (t2 = 19.5 ± 4.9 seconds, F = 11.88, P = 0.0012) were increased in the intervention group at t2. A significant difference was observed in the intervention group for the sing-loud SPL from t0 to t1 (t1 = 14.2 ± 1.7 dBA, F = 6.837, P = 0.0024). No difference was observed for the SPL and speak-loud SPL between the two groups. Figure 3 shows a comparison of the results of the two groups.