NRR:首都医科大学刘佳团队揭示血清中p-α-syn可作为缺血性脑卒中后认知障碍的潜在生物标志物
撰写:李雨凝
缺血性脑卒中(IS)是最常见的脑血管疾病,由脑血管狭窄或闭塞引起的急性缺血缺氧和脑组织坏死所致,具有发病率高、死亡率高、致残率高的特点 [1]。脑卒中后认知障碍是许多IS患者的主要继发性损伤之一,但该疾病的早期诊断和干预仍然存在困难。α-突触核蛋白(α-syn)是一种与神经退行性病变和认知障碍密切相关的蛋白质 [2]。病理状态下,α-syn常在丝氨酸 129 处发生磷酸化(p-α-syn)并产生异常聚集,从而造成神经元损伤 [3 , 4]。已有研究发现,在 IS 动物模型中,α-syn和p-α-syn 水平均明显升高 A [5], 同时,已有研究发现脑卒中患者红细胞中α-syn水平明显升高。然而,病理性α-syn是否在缺血性脑卒中后认知障碍中的发生中发挥作用尚不清楚。同时,血清作为更便于检测的生物样本,血清中p-α-syn
水平的变化及其与脑卒中后认知障碍的关系尚不明确。
首都医科大学脑重大疾病研究院刘佳团队在《中国神经再生研究(英文)》(Neural Regeneration Research)于2025年第8期发表的研究发现,IS模型小鼠脑梗死区周围和慢性缺氧小鼠脑中,α-syn均发生磷酸化和病理性聚集。这表明缺氧是导致IS脑中α-syn病变的内在原因。同时,该研究发现临床IS患者血清中p-α-syn水平明显低于对照人群,且与认知水平呈正相关。因此,血清中的p-α-syn 具有成为卒中后认知功能障碍的生物标志物的潜在可能性。
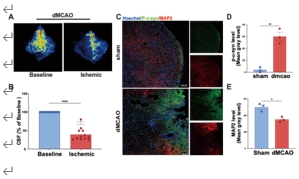
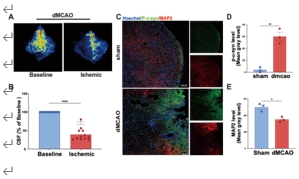
实验首先通过经典的远端大脑中动脉闭塞(dMCAO)手术建立
IS 小鼠模型,激光散斑结果显示血流显著减少证实造模成功(图1A,B),并对其大脑进行切片及免疫荧光染色,发现在梗死区周围神经元标志物MAP2显著减少的同时p-α-syn发生聚集(图1C-E)。这些结果表明,IS模型小鼠脑梗死区发生神经损伤并伴随p-α-syn的病理改变。
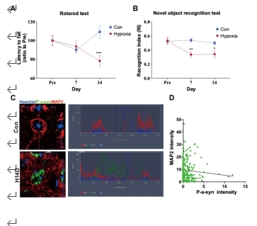
缺血性卒中是由于脑血管狭窄或闭塞导致的缺血缺氧性疾病,因此研究人员建立了慢性缺氧小鼠模型,转棒和新物体识别两项行为学检测表明慢性缺氧小鼠在缺氧14天时发生神经损伤(图2A,B),同时对其大脑切片进行免疫荧光染色,结果表明慢性缺氧会造成小鼠脑中神经损伤并伴随α-syn的磷酸化及聚集,而且神经元数量与脑中p-α-syn水平呈负相关(图2C,D)。综上所述,缺氧是导致IS小鼠脑中α-syn发生病理性改变的关键因素。
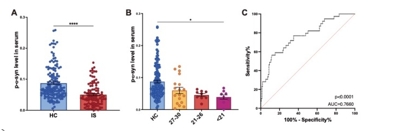
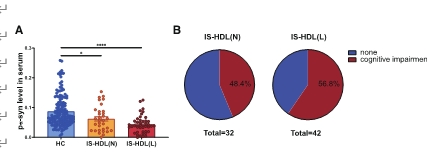
同时,该研究还纳入了临床患者的血清样本,对临床血清样本使用ELISA方法检测血清中p-α-syn水平的变化发现IS患者血清中p-α-syn水平显著低于对照组(图3A)。这提示p-α-syn可能具有成为脑卒中继发性脑损伤生物标志物的潜力。为了确定血清p-α-syn水平的变化是否预示着卒中后认知障碍的发生,研究者进一步分析了IS患者血清p-α-syn水平与认知相关临床表现之间的相关性。收集IS患者的MMSE评分进行分析,通常MMSE 评分低于 27 分被认为发生了认知障碍。该研究的结果为IS患者血清中p-α-syn水平与其认知功能呈正相关(图3B)。用于区分对照组和卒中后认知障碍时,血清 p-α-syn 水平的 AUC 值为 0.7660 [95% CI:0.6798-0.8523],这表明血清 p-α-syn 具有成为卒中后认知障碍的生物标志物的潜力。
此外,此次研究也对血清p-α-syn的水平与其他生化指标间的相关性进行了分析,比较了多种生化指标,包括高密度脂蛋白、低密度质蛋白,总胆固醇和肌酐等,利用热图的形式显示每个指标之间的皮尔逊相关性,结果显示血清中p-α-syn的水平与高密度脂蛋白(HDL)呈正相关(图4)。同时,将IS患者分为HDL正常组(IS-HDL(C))和HDL水平较低组(IS-HDL(L))组,对其血清中p-α-syn水平进行比较,结果显示高密度质蛋白异常的IS患者血清中p-α-syn水平更低(图5)。接下来,研究者统计了不同高密度脂蛋白水平的IS患者卒中后认知障碍的发生率,结果显示, IS-HDL(L)组认知障碍的发生率更高(图5)。以上研究结果表明,高密度脂蛋白异常可能是导致IS患者血清p-α-syn水平下降并影响卒中后认知障碍发生率的一个因素。
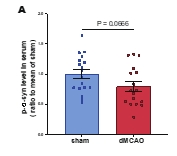
最后,研究者在IS模型小鼠上进行验证。IS模型小鼠在造模后14天时血清中p-α-syn水平相较于假手术组虽没有显著降低,但具有较明显的下降趋势(图6)。
#br#
图1 IS模型小鼠造模成功,且梗死区周围神经损伤伴随α-syn病理性聚集
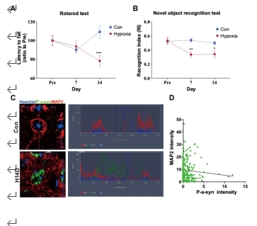
图2 慢性缺氧小鼠产生认知功能损伤,且脑中α-syn发生磷酸化及病理性聚集
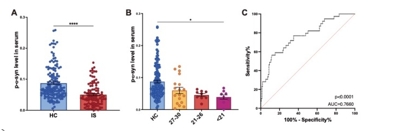
图3 IS患者血清中p-α-syn的水平明显低于对照人群,且与认知功能呈正相关

图4 IS患者血清中p-α-syn的水平与HDL呈正相关
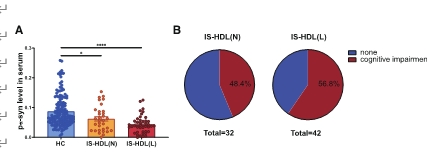
图5 高密度脂蛋白异常的IS患者血清中p-α-syn的水平更低,认知障碍发生率更高
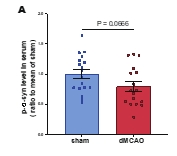
图6 IS模型小鼠在造模后14天血清中p-α-syn的水平具有下降趋势
总之,血清中p-α-syn的水平具有作为卒中后认知障碍的生物标志物的潜力,这为将来早期识别和干预该疾病提供了可能性,也为开发针对性的治疗方法提供了基础。同时,本研究的结果提示α-syn在发生神经损伤的脑中聚集,同时在血清中却显著降低。针对这一相反的现象,研究人员提出了一个假设:前期研究显示α-syn 可沿着动脉血管管壁被运出大脑 [6],因此猜想在生理情况下,作为一种“自我保护”机制,脑中有毒的、病理形式的p-α-syn会被排出;然而在缺血性卒中发生后,这种“自我保护”机制就失效了,p-α-syn无法排出进而沉积在大脑梗死区周围。当然,这一猜想仍需更多基础实验加以证实。此外,虽然该研究发现IS患者血清中p-α-syn的水平与HDL呈正相关,但仍需进一步证实。理想情况下,可利用高脂饮食合并IS造模的模型小鼠,对其进行相关指标的检测,以明确血清中p-α-syn的水平与HDL水平的关系。
图文摘要:
 #br#
#br#
在正常情况下,人体会主动将“有毒的” p-α-syn 从大脑排出到血中。然而,当缺血性卒中发生时,p-α-syn在梗死区周围沉积,无法排出,最终导致血液中其含量下降。
参考文献
[1] ADDIN EN.REFLIST Datta A, Sarmah D,
Mounica L, et
al. Cell death pathways in ischemic stroke and targeted
pharmacotherapy. Transl Stroke Res. 2020;11:1185-1202
[2]
Sorrentino
ZA, Giasson BI, Chakrabarty P. α-Synuclein and astrocytes: tracing the pathways
from homeostasis to neurodegeneration in Lewy body disease. Acta Neuropathol.
2019;138:1-21.
[3]
Fujiwara H, Hasegawa M,
Dohmae N, et
al. alpha-Synuclein is phosphorylated in synucleinopathy
lesions. Nat Cell Biol. 2002;4:160-164
[4]
Luk KC, Kehm V, Carroll
J, et
al. Pathological α-synuclein transmission initiates
Parkinson-like neurodegeneration in nontransgenic mice. Science. 2012;338:949-953.
[5]
Kim T, Mehta SL, Kaimal
B, et
al. Poststroke induction of α-synuclein mediates ischemic brain
damage. J Neurosci. 2016;36:7055-7065.
[6]
Nimmo J, Johnston DA,
Dodart JC, et
al. Peri-arterial pathways for clearance of alpha-Synuclein and
tau from the brain: Implications for the pathogenesis of dementias and for
immunotherapy. Alzheimers Dement (Amst). 2020;12:e12070.
#br#

 #br#
#br#