中国神经再生研究(英文版) ›› 2025, Vol. 20 ›› Issue (10): 3013-3024.doi: 10.4103/NRR.NRR-D-23-01651
新冠肺炎睡眠障碍患者存在持续性灰质结构异常:一项为期3个月的纵向研究
Persistent alterations in gray matter in COVID-19 patients experiencing sleep disturbances: a 3-month longitudinal study
Kaixuan Zhou1, 2, #, Gaoxiong Duan2, #, Ying Liu2 , Bei Peng2 , Xiaoyan Zhou2 , Lixia Qin3 , Lingyan Liang2 , Yichen Wei2 , Qingping Zhang2 , Xiaocheng Li2 , Haixia Qin2 , Yinqi Lai2 , Yian Lu3 , Yan Zhang2 , Jiazhu Huang2 , Jinli Huang2 , Yinfei Ouyang2 , Bolin Bin2 , Mingming Zhao3 , Jun Liu4, *, Jianrong Yang5, *, Demao Deng1, 2, *
- 1 Guangxi Key Laboratory of Special Biomedicine; School of Medicine, Guangxi University, Nanning, Guangxi Zhuang Autonomous Region, China; 2 Department of Radiology, the People’s Hospital of Guangxi Zhuang Autonomous Region, Guangxi Academy of Medical Sciences, Nanning, Guangxi Zhuang Autonomous Region, China; 3 Department of Sleep Medicine, the People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi Zhuang Autonomous Region, China; 4 Department of Radiology, The Second Xiangya Hospital, Central South University, Changsha, Hunan Province, China; 5 Guangxi Clinical Research Center for Sleep Medicine, the People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi Zhuang Autonomous Region, China
摘要:
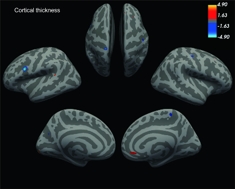
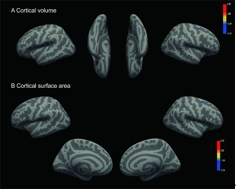
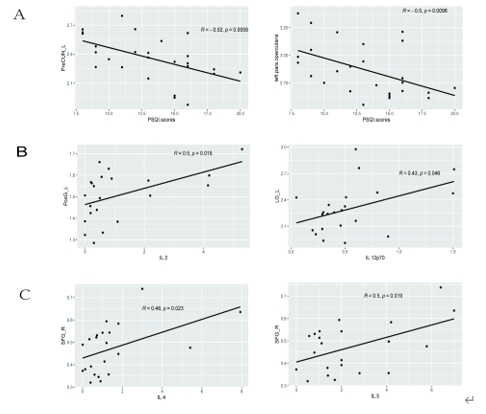
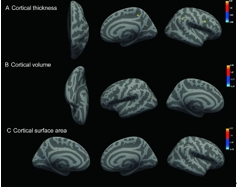
睡眠障碍是SARS-CoV-2感染康复者最常见的神经精神表现之一。既往一项纵向随访研究表明,从新冠肺炎中恢复的睡眠障碍患者的脑结构存在异常。然而,目前对新冠肺炎导致的睡眠障碍的神经影像学研究主要集中在长新冠中,尚缺乏急性感染期数据,这限制了对新冠肺炎导致的睡眠障碍的发病机制的了解。因此,这项纵向研究拟探索感染急性期患者的大脑结构是否发生变化,并通过3个月的随访观察其长期变化。研究共纳入26例患有睡眠障碍的新冠肺炎患者(51.5 ± 13.57岁,8女18男)、27例无睡眠障碍的新冠肺炎患者(47.33 ± 15.98岁,9女18男)和31名匹配的健康对照者(49.19 ± 17.51岁,9女22男),其中11例患有睡眠障碍的新冠肺炎患者在3个月进行纵向分析。结果发现,患有睡眠障碍的新冠肺炎患者几乎所有脑叶的结构都发生了变化,其中侧左额下回岛盖部和左侧楔前叶的皮质厚度与匹兹堡睡眠质量指数呈负相关。与健康对照组相比,新冠肺炎患者海马及其子区体积均发生了变化。3个月的纵向随访结果显示,与基线相比,患有睡眠障碍的新冠肺炎患者额顶叶皮质的大脑结构指数(皮质厚度、皮质灰质体积和皮质表面积)发生了变化。上述结果表明,新冠肺炎引起的睡眠障碍患者的脑结构异常始于感染急性期,且在3个月随访时持续存在。这填补了新冠急性期睡眠障碍患者神经影像证据的空白,有助于更好地理解新冠肺炎引起的睡眠障碍的病理机制。
https://orcid.org/0000-0002-7565-2607 (Demao Deng)