脑损伤
-
Figure 4|Pathological findings in patients with CV2/CRMP5 antibody-associated paraneoplastic neurological syndrome.
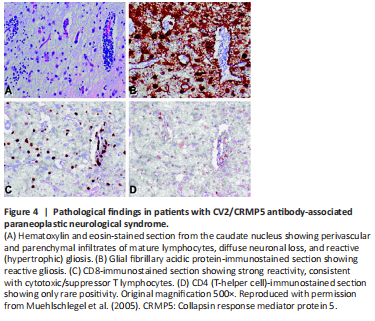
Regarding the pathology of CV2/CRMP5 antibody-associated PNS, perivascular and parenchymal T lymphocyte infiltration, neuronal loss, gliosis (Muehlschlegel et al., 2005; Figure 4), microglial activation, and rare microglial nodules formed by focal microglial hyperplasia (Cross et al., 2003) are seen in the brain and spinal cord. Cerebellar cortex atrophy and Purkinje cell decrease can be seen in the lesions that are restricted to the cerebellum (Vernino et al., 2002). One case study showed that the lymphocytic infiltrate within the parenchyma consisted exclusively of CD8+ T lymphocytes, whereas the perivascular infiltrate contained both B and T lymphocytes (CD4- and CD8-reactive; Muehlschlegel et al., 2005).
Figure 5|Optic disc photographs, fluorescein images, and vitreous biopsy.
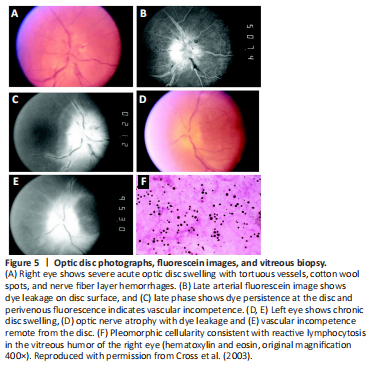
Cross et al. (2003) found that all but one of 15 patients with documented fundoscopy showed optic disc edema, commonly combined with hemorrhage of the nerve fiber layer, some with fan-shaped or diffuse atrophy of the optic disc. Fluorescence fundus angiography showed enhanced penetration and leakage of the optic papilla, and some cases had subretinal fluid and dye leakage from vessels distant from the optic disc, suggesting vascular insufficiency (Cross et al., 2003; Figure 5). Another study found that all 12 patients with ocular symptoms had optic disc edema in the fundus (Cohen et al., 2020).