NRR:首都医科大学附属北京潞河医院陈学明和张焱团队揭示人牙髓干细胞条件培养基促进脊髓损伤后神经功能恢复的机制
撰文:刘涛、马子谦、张焱、陈学明
脊髓损伤是一种严重的中枢系统创伤性疾病,目前尚无确切治疗方法[1]。脊髓损伤急性期发生的复杂的微环境失衡是导致其难以治愈的重要原因[2]。细胞焦亡是一种程序性的细胞死亡,发生在脊髓损伤急性期,可引发剧烈炎症反应,加重微环境失衡[3]。小胶质细胞是中枢神经系统固有免疫细胞,是脊髓损伤后发生焦亡的主要细胞类型。既往研究表明,抑制小胶质细胞焦亡可减轻脊髓损伤,促进功能恢复[4]。牙髓干细胞是一种来源于颅神经嵴的干细胞,与脊髓在胚胎时期同源,因此成为更佳的细胞选择[5]。干细胞移植治疗面临致畸、细胞存活率低等难题,其旁分泌产物,如外泌体、条件培养基治疗脊髓损伤越来越受到关注。已有研究证实,牙源性干细胞条件培养基可促进脊髓损伤鼠的功能恢复[6]。但关于牙髓干细胞条件培养基是否可通过抑制小胶质细胞焦亡减轻脊髓损伤尚缺乏研究。
来自中国首都医科大学附属北京潞河医院陈学明和张焱团队在《中国神经再生研究(英文版)》(Neural Regeneration Research)上发表了题为“Conditioned medium from human dental pulp stem cells treats spinal cord injury by inhibiting microglial pyroptosis”的研究。结果发现,牙髓干细胞条件培养基可明显促进脊髓损伤大鼠运动功能及电传导功能的恢复。进一步研究证实,牙髓干细胞条件培养基发挥作用可能是通过抑制NLRP3/Caspase-1/白细胞介素1β通路减轻小胶质细胞焦亡实现的。这一研究提示,条件培养基是一种能穿越血脑屏障的生物制品,其未来可能在创伤性脊髓损伤急性期的治疗中起到重要的作用。
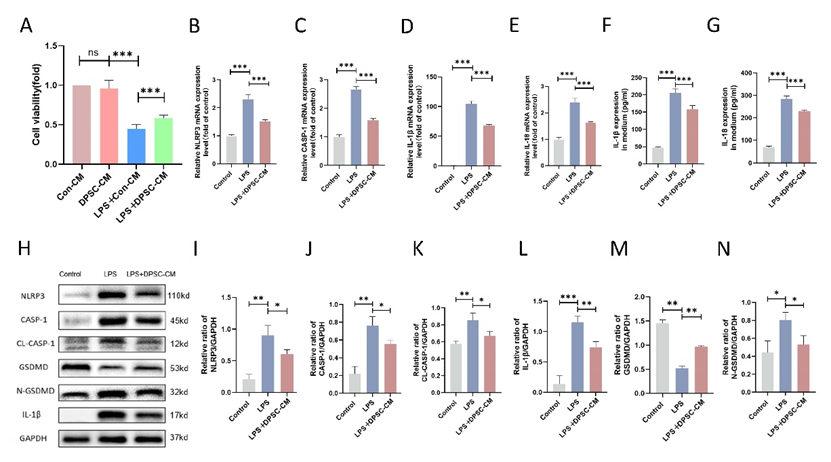
脊髓损伤后,小胶质细胞会发生焦亡,继而引发剧烈的炎症反应[7]。陈学明和张焱等首先在体外实验中从蛋白和基因两个层面证实了牙髓干细胞条件培养基可减轻脂多糖诱导的BV2细胞焦亡。脂多糖刺激BV2细胞系后,细胞活性下降,而牙髓干细胞条件培养基可提高细胞生存活性。脂多糖刺激后,焦亡的执行蛋白GSDMD表达升高,且牙髓干细胞条件培养基可逆转该趋势。
LRP3/Caspase-1/白细胞介素1β也表现出同样的趋势(图1)。这些结果表明,牙髓干细胞条件培养基具有抑制焦亡、抗炎特性。
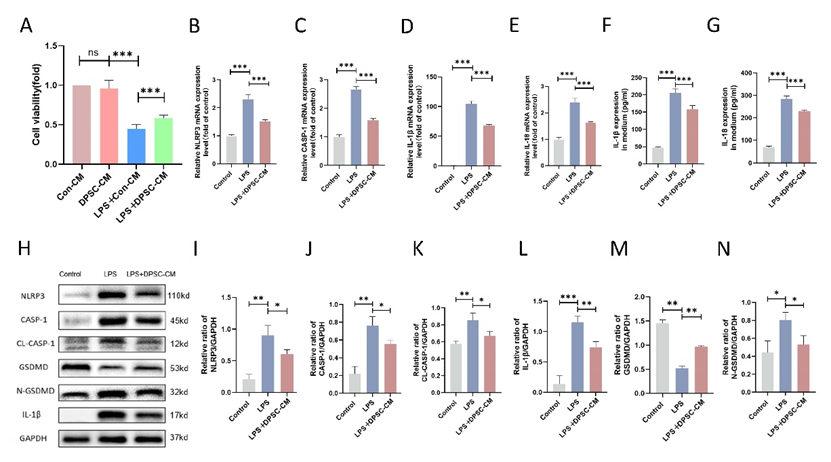
图1牙髓干细胞条件培养基可抑制脂多糖诱导的BV2细胞焦亡(图源:Liu et al., Neural Regen Res, 2024)
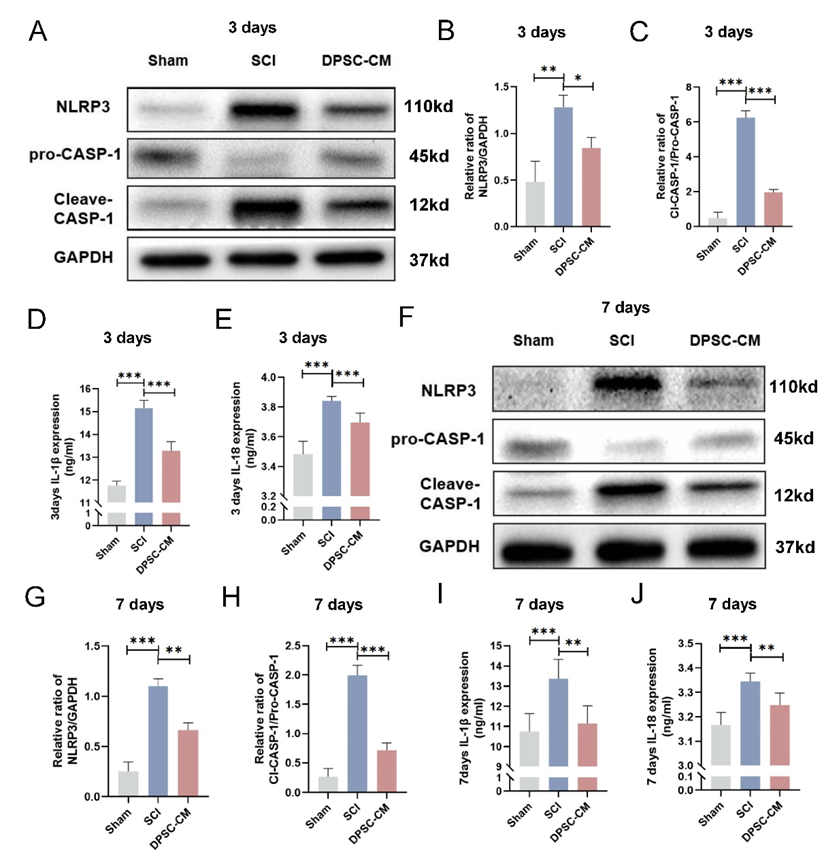
以往研究显示,减轻小胶质细胞焦亡可促进脊髓损伤大鼠功能恢复[8]。陈学明和张焱等将牙髓干细胞条件培养基与未培养牙髓干细胞的培养基分别腹腔注射治疗脊髓损伤大鼠,可见牙髓干细胞条件培养基能显著提供脊髓损伤大鼠的BBB评分与斜板实验评分,并改善其神经传导功能。进一步实验发现脊髓损伤后,NLRP3/Caspase-1/白细胞介素1β信号通路可在体内激活,且3种蛋白表达升高,而经牙髓干细胞条件培养基治疗后,该通路收到抑制(图2)。
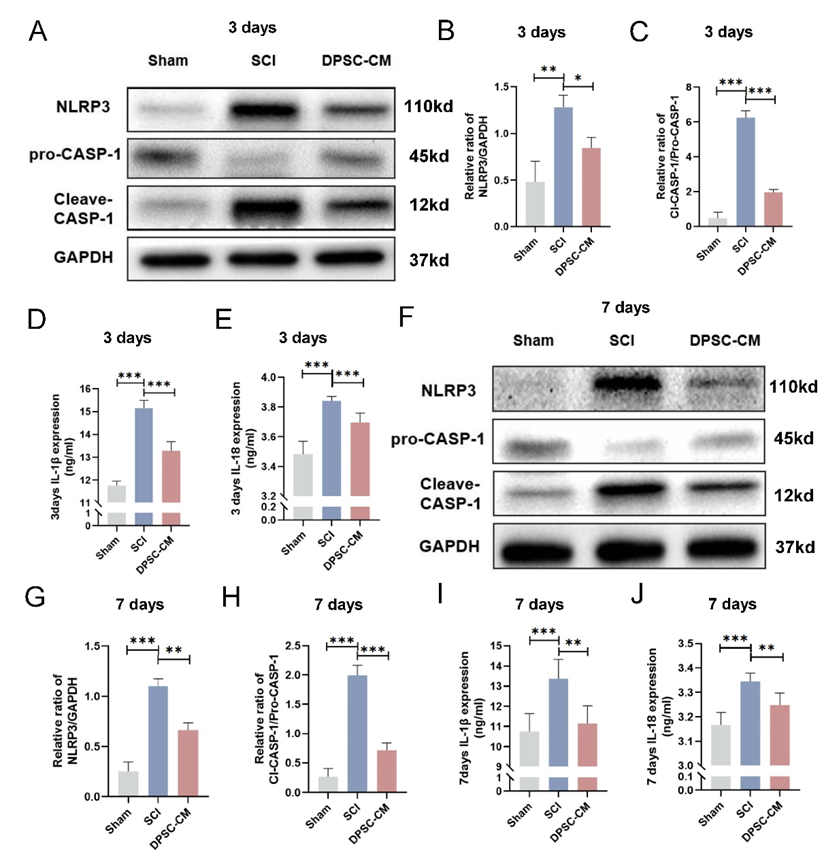
图2牙髓干细胞条件培养基抑制可脊髓损伤大鼠脊髓组织中NLRP3/Caspase-1/白细胞介素1β通路的激活(图源:Liu et al., Neural Regen Res, 2024)
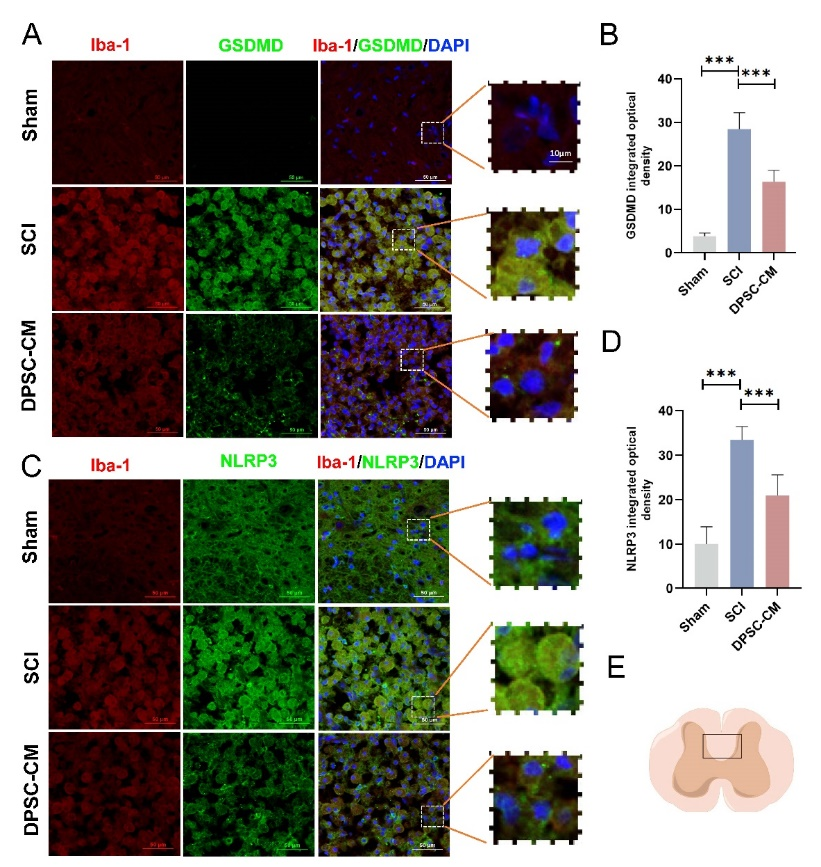
为验证是否抑制了小胶质细胞焦亡,陈学明和张焱等将焦亡相关通路标志物与小胶质细胞标志物离子钙结合衔接分子 1(Iba-1)免疫荧光共染色,结果显示,在脊髓损伤急性期,小胶质细胞中GSDMD表达明显增加,且发生焦亡,同时NLRP3/Caspase-1/白细胞介素1β信号通路被激活,而牙髓干细胞条件培养基治疗可改善这一趋势(图3)。以上研究结果说明,牙髓干细胞条件培养基可通过抑制NLRP3/Caspase-1/白细胞介素1β信号通路减轻小胶质细胞焦亡,从而促进脊髓损伤大鼠功能恢复。
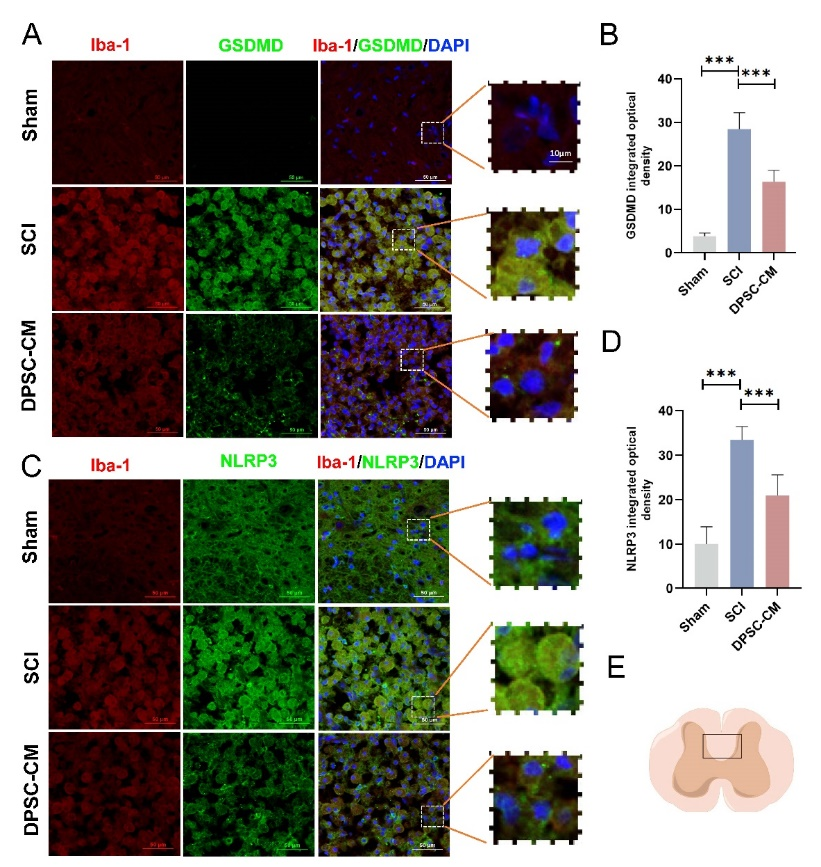
图3牙髓干细胞条件培养基可通过抑制NLRP3/Caspase-1/白细胞介素1β通路减轻小胶质细胞的焦亡(图源:Liu et al., Neural Regen Res, 2024)
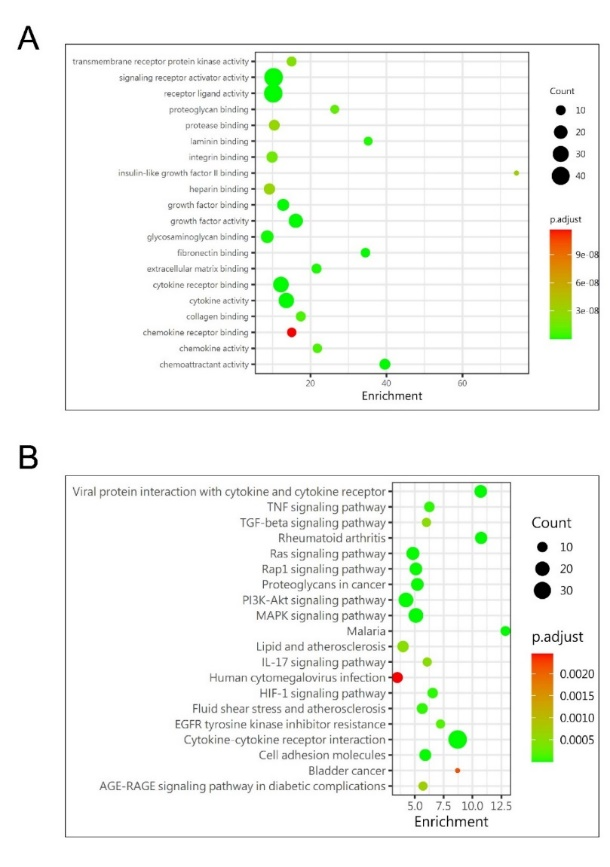
为进一步明确牙髓干细胞条件培养基疗效的原因,陈学明和张焱等将牙髓干细胞条件培养基与未培养牙髓干细胞的培养基进行了质谱分析,结果显示共有158种差异表达的蛋白。进一步对差异表达的蛋白进行KEGG分析发现,富集差异蛋白的通路主要为PI3K/AKT通路与MAPK通路。考虑到PI3K/AKT通路与细胞生存和迁移的关系更为密切,实验对相关蛋白进行了进一步分析,结果发现VEGF、HGF、ANG-1是含量最高的3种蛋白(图4)。据此提出可能是牙髓干细胞分泌的某种因子通过调控PI3K/AKT通路抑制了小胶质细胞的焦亡。
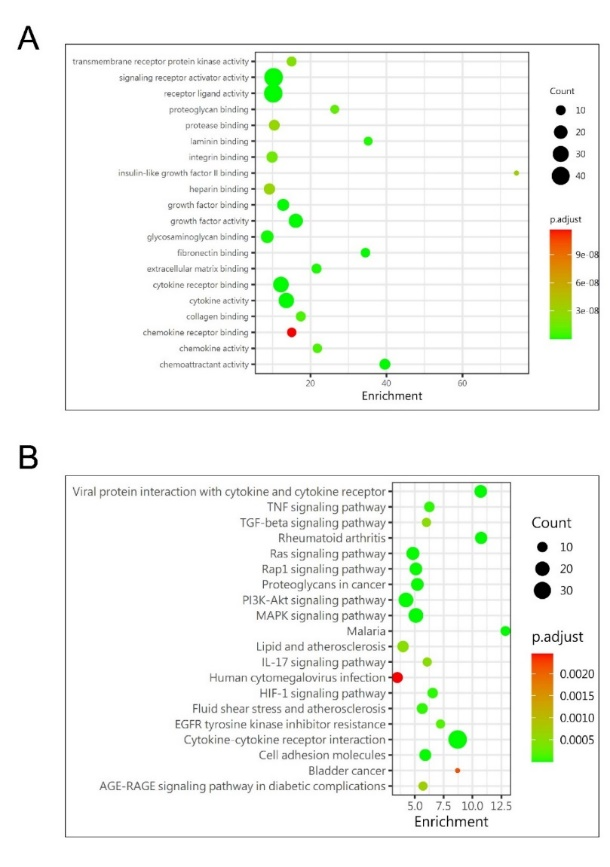
图4牙髓干细胞条件培养基质谱分析GO和KEGG结果(图源:Liu et al., Neural Regen Res, 2024)
综上所述,小胶质细胞焦亡在脊髓损伤继发性损伤中发挥重要的作用。牙髓干细胞条件培养基可能通过抑制NLRP3/Caspase-1/白细胞介素1β信号通路,在体外保护BV2细胞免受脂多糖诱导的焦亡。重要的是,牙髓干细胞条件培养基可减轻小胶质细胞焦亡,促进轴突再生和髓鞘形成,减少体内胶质瘢痕的形成,从而限制继发性损伤,进而促进脊髓损伤大鼠的功能恢复。因此,人牙髓干细胞条件培养基可能具有很好的脊髓损伤治疗潜力,这提示了一种治疗脊髓损伤的新策略。
由于实验使用BV2细胞系代替原代小胶质细胞,虽然BV2细胞系在大多数实验中已被证明是小胶质细胞的有效替代品,但仍有学者怀疑该细胞系不能完全替代小胶质细胞的作用[9, 10]。由于牙髓干细胞条件培养基成分复杂,虽实验已对其成分进行了质谱分析,但还需进一步证实是哪种成分发挥了作用。
原文链接:https://doi.org/10.4103/1673-5374.385309
参考文献
[1] Khorasanizadeh M, Yousefifard M, Eskian M, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine. 2019;doi: 10.3171/2018.10.SPINE18802.
[2] Fan B, Wei Z, Feng S. Progression in translational research on spinal cord injury based on microenvironment imbalance. Bone Res. 2022;10(1):35.
[3] Al Mamun A, Wu Y, Monalisa I, et al. Role of pyroptosis in spinal cord injury and its therapeutic implications. J Adv Res. 2021;28:97-109.
[4] Zhao H, Wang X, Liu S, et al. Paeonol regulates NLRP3 inflammasomes and pyroptosis to alleviate spinal cord injury of rat. BMC Neurosci. 2022;23(1):16.
[5] Gronthos S, Mankani M, Brahim J, et al. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A. 2000;97(25):13625-13630.
[6] Asadi-Golshan R, Razban V, Mirzaei E, et al. Sensory and motor behavior evidences supporting the usefulness of conditioned medium from dental pulp-derived stem cells in spinal cord injury in rats. Asian Spine J. 2018;12(5):785-793.
[7] Mckenzie BA, Dixit VM, Power C. Fiery cell death: pyroptosis in the central nervous system. Trends Neurosci. 2020;43(1):55-73.
[8] Wu C, Chen H, Zhuang R, et al. Betulinic acid inhibits pyroptosis in spinal cord injury by augmenting autophagy via the AMPK-mTOR-TFEB signaling pathway. Int J Biol Sci. 2021;17(4):1138-1152.
[9] Henn A, Lund S, Hedtjärn M, et al. The suitability of BV2 cells as alternative model system for primary microglia cultures or for animal experiments examining brain inflammation. ALTEX. 2009;26(2):83-94.
[10] Xu Y, Hu X, Li F, et al. GDF-11 protects the traumatically injured spinal cord by suppressing pyroptosis and necroptosis via TFE3-mediated autophagy augmentation. Oxid Med Cell Longev. 2021;2021:8186877.

第一作者:刘涛,首都医科大学在读硕士,师从陈学明教授,研究方向为脊髓损伤基础研究。

第一作者:马子谦,首都医科大学在读硕士,师从陈学明教授,研究方向为脊髓损伤基础研究。

通讯作者:张焱,医学博士,毕业于天津医科大学、香港中文大学,师从全国著名脊柱外科专家,教育部长江学者特聘教授冯世庆教授、神经发育学专家陈活彝教授。研究方向为脊髓损伤与神经再生基础研究。

通讯作者:陈学明,主任医师、副教授、硕士研究生导师,首都医科大学附属北京潞河医院副院长,脊柱外科学科带头人。研究方向为颈腰椎退变性疾病与脊柱脊髓损伤。主持多项市区级课题。中国康复医学会脊柱脊髓专业委员会委员。